Overview
This new Guidelines summary covers the assessment, treatment, and management of depression in people aged 18 years and over.
This summary does not cover recommendations on:
- behavioural couples therapy for depression
- preventing relapse
- chronic depressive symptoms
- depression in people with a diagnosis of personality disorder
- psychotic depression
- electroconvulsive therapy for depression
- transcranial magnetic stimulation for depression
- implanted vagus nerve stimulation for treatment-resistant depression
- access, coordination and delivery of care.
Recognition and Assessment
- Be alert to possible depression (particularly in people with a past history of depression or a chronic physical health problem with associated functional impairment) and consider asking people who may have depression if:
- During the last month, have they often been bothered by feeling down, depressed or hopeless?
- During the last month, have they often been bothered by having little interest or pleasure in doing things?See also the NICE guideline on depression in adults with a chronic physical health problem.
- If a person answers ‘yes’ to either of the depression identification questions (see the first recommendation in this section) but the practitioner is not competent to perform a mental health assessment, refer the person to an appropriate professional who can. If this professional is not the person’s GP, inform the person’s GP about the referral.
- If a person answers ‘yes’ to either of the depression identification questions (see the first recommendation in this section) and the practitioner is competent to perform a mental health assessment, review the person’s mental state and associated functional, interpersonal and social difficulties.
- Consider using a validated measure (for example, for symptoms, functions and/or disability) when assessing a person with suspected depression to inform and evaluate treatment.
- If a person has language or communication difficulties (for example, sensory or cognitive impairments or autism), to help identify possible depression consider:
- asking the person about their symptoms directly, using an appropriate method of communication depending on the person’s needs (for example, using a British Sign Language interpreter, English interpreter, or augmentative and alternative communication)
- asking a family member or carer about the person’s symptoms.See also the NICE guideline on mental health problems in people with learning disabilities and the NICE guideline on autism spectrum disorder.
Initial Assessment
- Conduct a comprehensive assessment that does not rely simply on a symptom count when assessing a person who may have depression, but also takes into account severity of symptoms, previous history, duration and course of illness. Also, take into account both the degree of functional impairment and/or disability associated with the possible depression and the length of the episode.
- Discuss with the person how the factors below may have affected the development, course and severity of their depression in addition to assessing symptoms and associated functional impairment:
- any history of depression and coexisting mental health or physical disorders
- any history of mood elevation (to determine if the depression may be part of bipolar disorder); see the NICE guideline on bipolar disorder
- any past experience of, and response to, previous treatments
- personal strengths and resources, including supportive relationships
- difficulties with previous and current interpersonal relationships
- current lifestyle (for example, diet, physical activity, sleep)
- any recent or past experience of stressful or traumatic life events, such as redundancy, divorce, bereavement, trauma (also see the NICE guideline on post-traumatic stress disorder)
- living conditions, drug (prescribed or illicit) and alcohol use, debt, employment situation, loneliness and social isolation.
Risk Assessment and Management
- Always ask people with depression directly about suicidal ideation and intent. If there is a risk of self-harm or suicide:
- assess whether the person has adequate social support and is aware of sources of help
- arrange help appropriate to the level of need
- advise the person to seek further help if the situation deteriorates.
- If a person with depression presents considerable immediate risk to themselves or others, refer them urgently to specialist mental health services.
- Advise people with depression of the potential for increased agitation, anxiety and suicidal ideation in the initial stages of treatment. Check if they have any of these symptoms and:
- ensure that the person knows how to seek help promptly
- review the person’s treatment if they develop marked and/or prolonged agitation.
- Advise a person with depression and their family or carer to be vigilant for mood changes, agitation, negativity and hopelessness, and suicidal ideation, and to contact their practitioner if concerned. This is particularly important during high-risk periods, such as starting or changing treatment and at times of increased personal stress.
- If a person with depression is assessed to be at risk of suicide:
- do not withhold treatment for depression on the basis of their suicide risk
- take into account toxicity in overdose if an antidepressant is prescribed, or the person is taking other medication, and if necessary limit the amount of medicine available
- consider increasing the level of support provided, such as more frequent in-person, video call or telephone contact
- consider referral to specialist mental health services.For further advice on risk assessment, see the NICE guideline on self-harm. For further advice on medication, see the recommendations on antidepressant medication for people at risk of suicide.
Choice of Treatments
- Discuss with people with depression:
- what, if anything, they think might be contributing to the development of their depression (see recommendation 1.2.7 in the full guideline)
- whether they have ideas or preferences about starting treatment, and what treatment options they have previously found helpful or might prefer
- their experience of any prior episodes of depression, or treatments for depression
- what they hope to gain from treatment.
- Allow adequate time for the initial discussion about treatment options, and involve family members, carers or other supporters if agreed by the person with depression.
- Help build a trusting relationship with the person with depression and facilitate continuity of care by:
- ensuring they can see the same healthcare professional wherever possible
- recording their views and preferences so that other practitioners are aware of these details.
- Discuss with people with depression their preferences for treatments (including declining an offer of treatment, or changing their mind once a treatment has started) by providing:
- information on what treatments are NICE-recommended, their potential benefits and harms, any waiting times for treatments, and the expected outcomes (see table 1 and table 2 in the full guideline on the recommended treatments for a new episode of less severe and more severe depression)
- a choice of:
- the treatments recommended in this guideline
- how they will be delivered (for example individual or group, in person or remotely) and
- where they will be delivered
- the option to attend with a family member or friend when possible, for some or all of their treatment
- the option to express a preference for the gender of the healthcare professional, to see a professional they already have a good relationship with, or to change professional if the relationship is not working.
- Make a shared decision with the person about their treatment. See the NICE guideline on shared decision making.
- Commissioners and service managers should ensure that people can express a preference for NICE-recommended treatments, that those treatments are available in a timely manner, particularly in severe depression, and that they are monitored to ensure equality of access, provision, outcomes and experience.
Delivery of Treatments
All Treatments
- When considering treatments for people with depression:
- carry out an assessment of need
- develop a treatment plan
- take into account any physical health problems
- take into account any coexisting mental health problems
- discuss what factors would make the person most likely to engage with treatment (including reviewing positive and negative experiences of previous treatment)
- take into account previous treatment history
- address any barriers to the delivery of treatments because of any disabilities, language or communication difficulties
- ensure regular liaison between healthcare professionals in specialist and non-specialist settings, if the person is receiving specialist support or treatment.For people with depression who also have learning disabilities, see the NICE guideline on mental health problems in people with learning disabilities. For people with depression who also have autism, see the NICE guideline on autism spectrum disorder. For people with depression who also have dementia, see the NICE guideline on dementia. For people with depression in pregnancy or the postnatal period, or who are breastfeeding, see the NICE guideline on antenatal and postnatal mental health. For people with depression who are menopausal, see the NICE guideline on menopause. For people with depression and physical health problems, see the NICE guideline on depression in adults with a chronic physical health problem and also see the recommendations on collaborative care in the full guideline.
- Match the choice of treatment to meet the needs and preferences of the person with depression. Use the least intrusive and most resource efficient treatment that is appropriate for their clinical needs, or one that has worked for them in the past.
- For all people with depression having treatment:
- review how well the treatment is working with the person between 2 and 4 weeks after starting treatment
- monitor and evaluate treatment concordance
- monitor for side effects and harms of treatment
- monitor suicidal ideation, particularly in the early weeks of treatment (see also the recommendations on antidepressant medication for people at risk of suicide, and the recommendations on risk assessment in the full guideline)
- consider routine outcome monitoring (using appropriate validated sessional outcome measures, for example PHQ-9) and follow up.
Pharmacological Treatments
Starting Antidepressant Medication
- When offering a person medication for the treatment of depression, discuss and agree a management plan with the person. Include:
- the reasons for offering medication
- the choices of medication (if a number of different antidepressants are suitable)
- the dose, and how the dose may need to be adjusted
- the benefits, covering what improvements the person would like to see in their life and how the medication may help
- the harms, covering both the possible side effects and withdrawal effects, including any side effects they would particularly like to avoid (for example, weight gain, sedation, effects on sexual function)
- any concerns they have about taking or stopping the medication (also see the recommendations on stopping medication in the full guideline).Make sure they have written information to take away and to review that is appropriate for their needs.
- When prescribing antidepressant medication, ensure people have information about:
- how they may be affected when they first start taking antidepressant medication, and what these effects might be
- how long it takes to see an effect (usually, if the antidepressant medication is going to work, within 4 weeks)
- when their first review will be; this will usually be within 2 weeks to check their symptoms are improving and for side effects, or after 1 week if a new prescription is for a person aged 18 to 25 years or if there is a particular concern for risk of suicide (see recommendations on antidepressant medication for people at risk of suicide in the full guideline)
- the importance of following instructions on how to take antidepressant medication (for example, time of day, interactions with other medicines and alcohol)
- why regular monitoring is needed, and how often they will need to attend for review
- how they can self-monitor their symptoms, and how this may help them feel involved in their own recovery
- that treatment might need to be taken for at least 6 months after the remission of symptoms, but should be reviewed regularly
- how some side effects may persist throughout treatment
- withdrawal symptoms and how these withdrawal effects can be minimised (see also the recommendations on stopping antidepressant medication).
- For further advice on safe prescribing of antidepressants, see the NICE guideline on medicines associated with dependence or withdrawal symptoms: safe prescribing and withdrawal management for adults. For further advice on the safe and effective use of medicines for people taking 1 or more medicines, see the NICE guideline on medicines optimisation.
Stopping Antidepressant Medication
- Advise people taking antidepressant medication to talk with the person who prescribed their medication (for example, their primary healthcare or mental health professional) if they want to stop taking it. Explain that it is usually necessary to reduce the dose in stages over time (called ‘tapering’) but that most people stop antidepressants successfully.
- Advise people taking antidepressant medication that if they stop taking it abruptly, miss doses or do not take a full dose, they may have withdrawal symptoms. Also advise them that withdrawal symptoms do not affect everyone, and can vary in type and severity between individuals.
For recommendations on antidepressant medication for older people, use of lithium as augmentation, use of oral antipsychotics as augmentation, use of St John’s Wort, and physical treatments and activities, including light therapy and activities to help wellbeing, refer to the full guideline.
Treatment for a New Episode of Less Severe Depression
In this guideline, the term less severe depression includes the traditional categories of subthreshold symptoms and mild depression.
For recommendations on active monitoring in people who do not want treatment, refer to the full guideline.
Treatment Options
- Discuss treatment options with people with a new episode of less severe depression, and match their choice of treatment to their clinical needs and preferences:
- use table 1 in the full guideline and the visual summary (Algorithm 1) to guide and inform the conversation
- take into account that all treatments in table 1 can be used as first-line treatments, but consider the least intrusive and least resource intensive treatment first (guided self-help)
- reach a shared decision on a treatment choice appropriate to the person’s clinical needs, taking into account their preferences (see also the recommendations on choice of treatments)
- recognise that people have a right to decline treatment.
- Do not routinely offer antidepressant medication as first-line treatment for less severe depression, unless that is the person’s preference.
Algorithm 1: Depression in Adults: Discussing First-line Treatments for Less Severe Depression
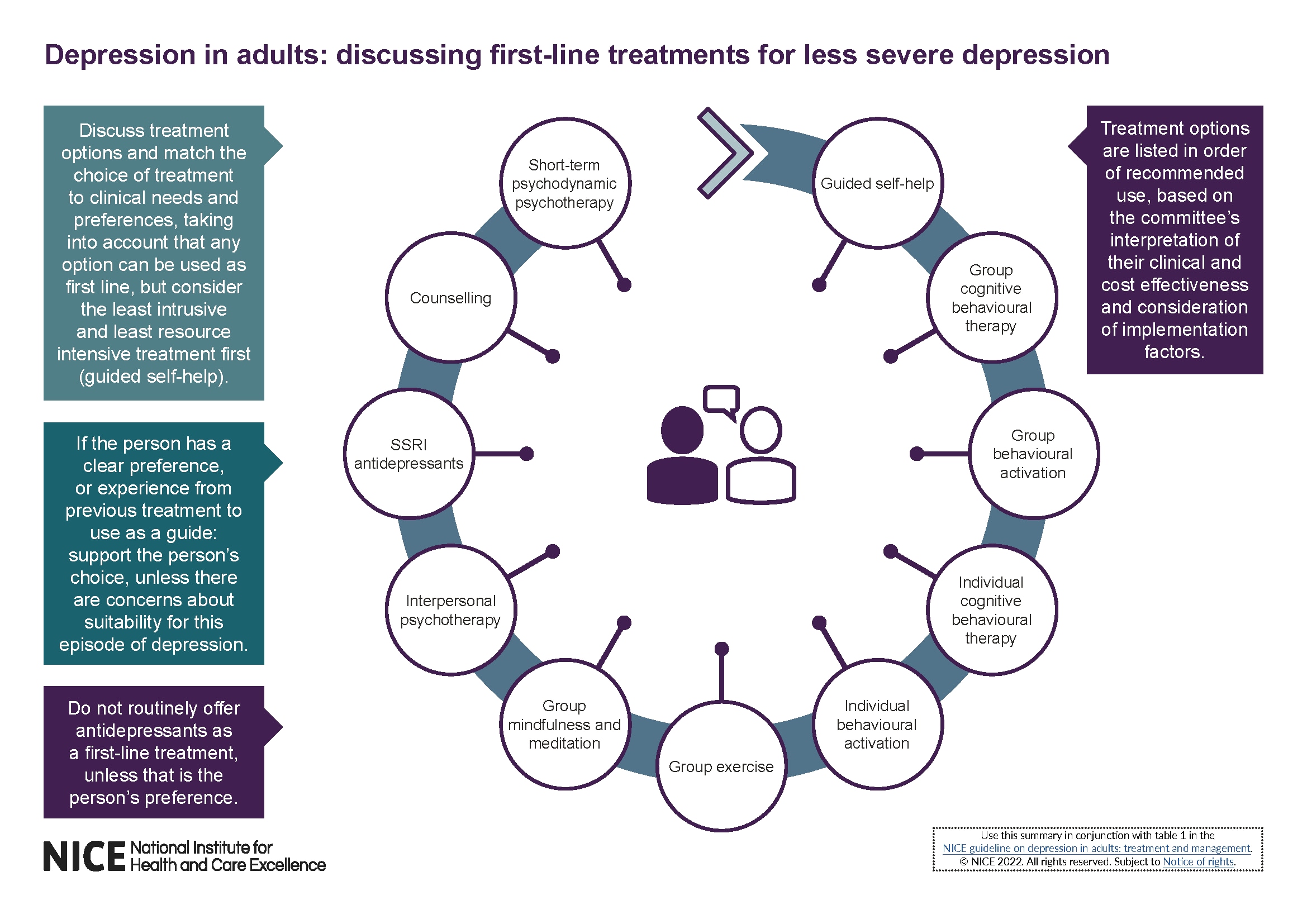
© NICE, 2022. All rights reserved. Subject to Notice of rights.
Treatment for a New Episode of More Severe Depression
In this guideline the term more severe depression includes the traditional categories of moderate and severe depression.
Treatment Options
- Discuss treatment options with people who have a new episode of more severe depression, and match their choice of treatment to their clinical needs and preferences:
- use table 2 in the full guideline and the visual summary (Algorithm 2) to guide and inform the conversation
- take into account that all treatments in table 2 can be used as first-line treatments
- reach a shared decision on a treatment choice appropriate to the person’s clinical needs, taking into account their preferences (see also the recommendations on choice of treatments)
- recognise that people have a right to decline treatment.
Algorithm 2: Depression in Adults: Discussing First-line Treatments for More Severe Depression
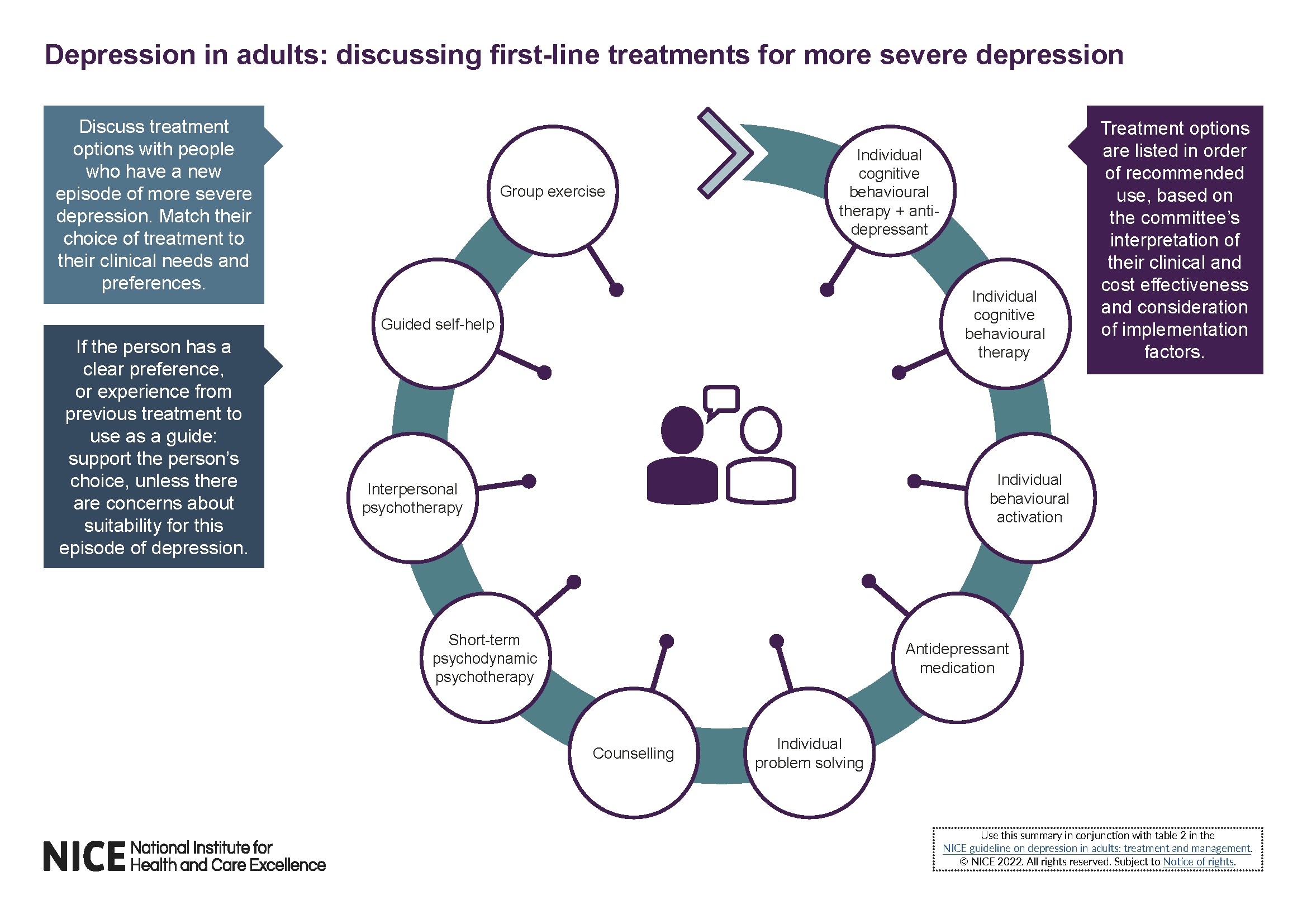
For recommendations on behavioural couples therapy for depression and preventing relapse, refer to the full guideline.
Further-line Treatment
Algorithm 3: Depression in Adults: Further-line Treatment
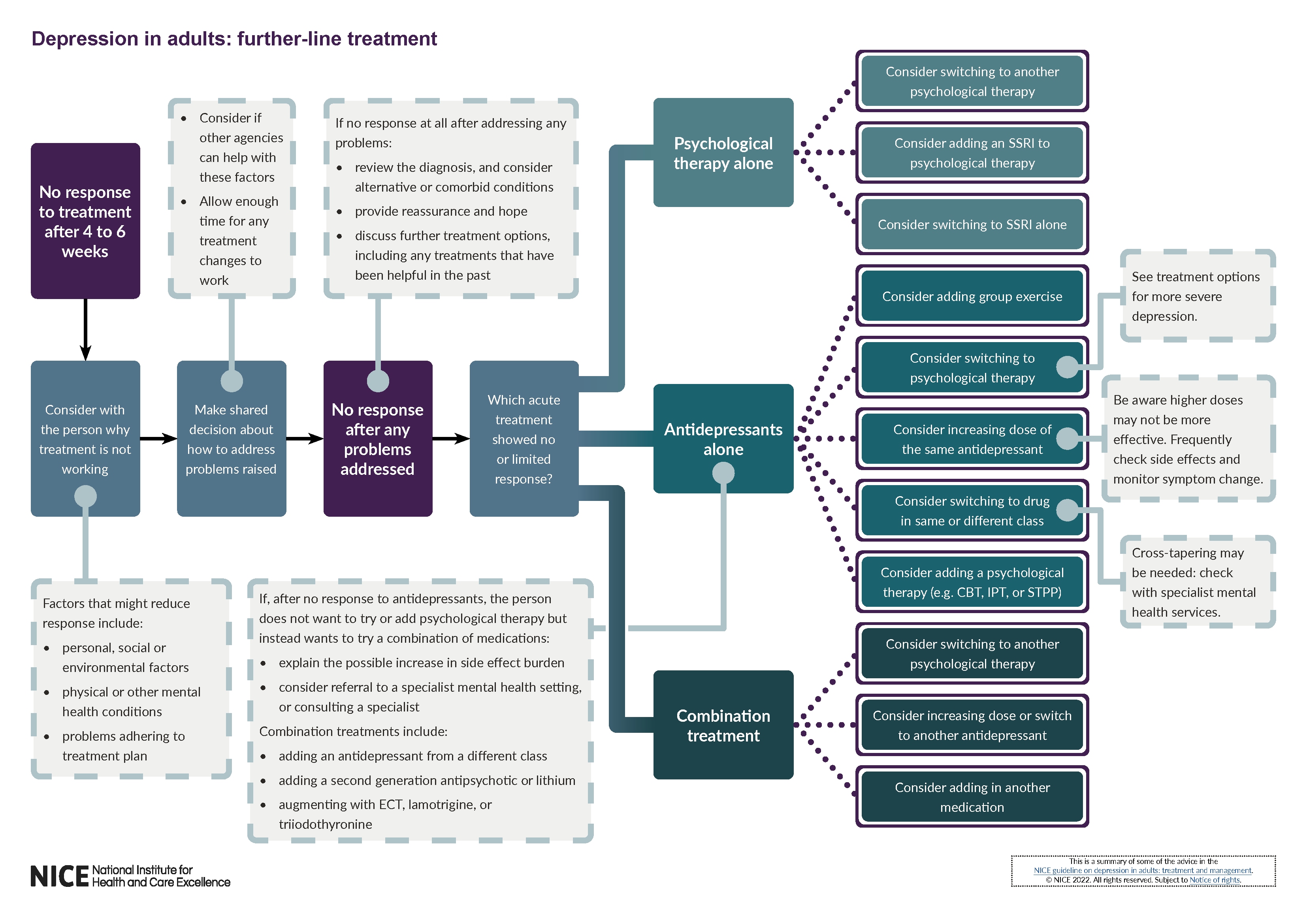
© NICE, 2022. All rights reserved. Subject to Notice of rights.
- If a person’s depression has not responded at all after 4 weeks of antidepressant medication at a recognised therapeutic dose, or after 4 to 6 weeks for psychological therapy or combined medication and psychological therapy, discuss with them:
- whether there are any personal, social or environmental factors or physical or other mental health conditions that might explain why the treatment is not working
- whether they have had problems adhering to the treatment plan (for example, stopping or reducing medication because of side effects, or missing sessions with their therapist).If any of these are the case, make a shared decision with the person about the best way to try and address any problems raised, including how other agencies may be able to help with these factors. See the visual summary on further-line treatment (Algorithm 3).
- If a person’s depression has not responded to treatment after addressing any problems raised (see the first recommendation in this section), and allowing an adequate time for treatment changes to work, review the diagnosis and consider the possibility of alternative or comorbid conditions that may limit response to depression treatments.
- Reassure the person that although treatment has not worked, other treatments can be tried, and may be effective.
- If a person’s depression has had no or a limited response to treatment with psychological therapy alone, and no obvious cause can be found and resolved, discuss further treatment options with the person (including what other treatments they have found helpful in the past) and make a shared decision on how to proceed based on their clinical need and preferences. Options include:
- switching to an alternative psychological treatment
- adding an SSRI to the psychological therapy
- switching to an SSRI alone.
- If a person’s depression has had no or a limited response to treatment with antidepressant medication alone, and no obvious cause can be found and resolved, discuss further treatment options with the person and make a shared decision on how to proceed based on their clinical need and preferences. Options include:
- adding a group exercise intervention
- switching to a psychological therapy (see the suggested treatment options for more severe depression)
- continuing antidepressant therapy by either increasing the dose or changing the drug. For example, by:
- increasing the dose of the current medication (within the licensed dose range) if the medication is well tolerated; be aware that higher doses of antidepressants may not be more effective and can increase the frequency and severity of side effects; ensure follow-up and frequent monitoring of symptoms and side effects after dose increases.
- switching to another medication in the same class (for example, another SSRI)
- switching to a medication of a different class (for example, an SSRI, SNRI, or in secondary care a TCA or MAOI); take into account that:
- switching medication may mean cross-tapering is needed; see the NICE clinical knowledge summary on switching antidepressants
- switching to or from an MAOI, or from one MAOI to another, will need to take place in, or with advice from, secondary care
- TCAs are dangerous in overdose, although lofepramine has the best safety profile
- changing to a combination of psychological therapy (for example, CBT, interpersonal psychotherapy [IPT] or STPP) and medication.Consider whether some of these decisions and treatments need other services to be involved (for example, specialist mental health services for advice on switching antidepressants).
- If a person’s depression has had no or a limited response to treatment with a combination of antidepressant medication and psychological therapy, discuss further treatment options with the person and make a shared decision on how to proceed based on their clinical need and preferences. Options include:
- switching to another psychological therapy
- increasing the dose or switching to another antidepressant (see the previous recommendation)
- adding in another medication (see the final recommendation in this section).
- Only consider vortioxetine when there has been no or limited response to at least 2 previous antidepressants. See the NICE technology appraisal guidance on the use of vortioxetine.
- If a person whose depression has had no response or a limited response to antidepressant medication does not want to try a psychological therapy, and instead wants to try a combination of medications, explain the possible increase in their side-effect burden.
- If a person with depression wants to try a combination treatment and is willing to accept the possibility of an increased side-effect burden (see the previous recommendation), consider referral to a specialist mental health setting or consulting a specialist. Treatment options include:
- adding an additional antidepressant medication from a different class (for example, adding mirtazapine or trazodone to an SSRI)
- combining an antidepressant medication with a second-generation antipsychotic (for example, aripiprazole, olanzapine, quetiapine or risperidone) or lithium
- augmenting antidepressants with electroconvulsive therapy (see the recommendations on electroconvulsive therapy for depression in the full guideline), lamotrigine, or triiodothyronine (liothyronine).Be aware that some combinations of classes of antidepressants are potentially dangerous and should be avoided (for example, a SSRI, SNRI or TCA with a MAOI), and that when using an antipsychotic the effects of this on depression, including loss of interest and motivation, should be carefully reviewed.In June 2022, this was an off-label use for some antipsychotics, lamotrigine, and triiodothyronine (liothyronine). See NICE’s information on prescribing medicines.
For recommendations on chronic depressive symptoms, depression in people with a diagnosis of personality disorder, psychotic depression, electroconvulsive therapy for depression, transcranial magnetic stimulation for depression, implanted vagus nerve stimulation for treatment-resistant depression, and access, coordination, and delivery of care, refer to the full guideline.

