This Guidelines summary covers the diagnosis and management of menopause, including in women who have premature ovarian insufficiency. The guideline aims to improve the consistency of support and information provided to women in menopause.
Individualised Care
- Adopt an individualised approach at all stages of diagnosis, investigation and management of menopause. Follow recommendations in the NICE guideline on patient experience in adult NHS services.
Diagnosis of Perimenopause and Menopause
- Diagnose the following without laboratory tests in otherwise healthy women aged over 45 years with menopausal symptoms:
- perimenopause based on vasomotor symptoms and irregular periods
- menopause in women who have not had a period for at least 12 months and are not using hormonal contraception
- menopause based on symptoms in women without a uterus
- Take into account that it can be difficult to diagnose menopause in women who are taking hormonal treatments, for example for the treatment of heavy periods
- Do not use the following laboratory and imaging tests to diagnose perimenopause or menopause in women aged over 45 years:
- anti-Müllerian hormone
- inhibin A
- inhibin B
- oestradiol
- antral follicle count
- ovarian volume
- Do not use a serum follicle-stimulating hormone (FSH) test to diagnose menopause in women using combined oestrogen and progestogen contraception or high-dose progestogen
- Consider using a FSH test to diagnose menopause only:
- in women aged 40 to 45 years with menopausal symptoms, including a change in their menstrual cycle
- in women aged under 40 years in whom menopause is suspected.
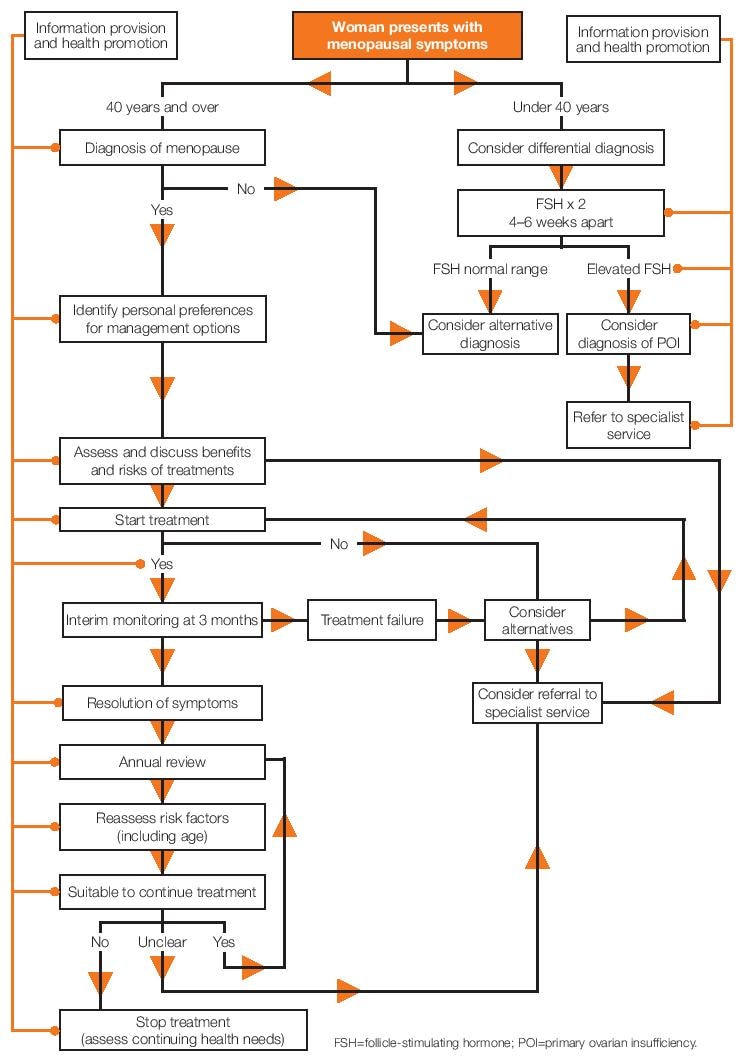
Care Algorithm
Information and Advice
- Give information to menopausal women and their family members or carers (as appropriate) that includes:
- an explanation of the stages of menopause
- common symptoms (see below) and diagnosis
- lifestyle changes and interventions that could help general health and wellbeing
- benefits and risks of treatments for menopausal symptoms
- long-term health implications of menopause
- Explain to women that as well as a change in their menstrual cycle they may experience a variety of symptoms associated with menopause, including:
- vasomotor symptoms (for example, hot flushes and sweats)
- musculoskeletal symptoms (for example, joint and muscle pain)
- effects on mood (for example, low mood)
- urogenital symptoms (for example, vaginal dryness)
- sexual difficulties (for example, low sexual desire)
- Give information to menopausal women and their family members or carers (as appropriate) about the following types of treatment for menopausal symptoms:
- hormonal, for example hormone replacement therapy (HRT)
- non-hormonal, for example clonidine
- non-pharmaceutical, for example cognitive behavioural therapy (CBT)
- Give information on menopause in different ways to help encourage women to discuss their symptoms and needs
- Give information about contraception to women who are in the perimenopausal and postmenopausal phase. See guidance from the Faculty of Sexual & Reproductive Healthcare on contraception for women aged over 40 years
- Offer women who are likely to go through menopause as a result of medical or surgical treatment (including women with cancer, at high risk of hormone-sensitive cancer or having gynaecological surgery) support and:
- information about menopause and fertility before they have their treatment
- referral to a healthcare professional with expertise in menopause.
Managing Short-term Menopausal Symptoms
- The recommendations in this section are not intended for women with premature ovarian insufficiency (see full guideline for management of premature ovarian insufficiency)
- Adapt a woman's treatment as needed, based on her changing symptoms.
Vasomotor Symptoms
- Offer women HRT for vasomotor symptoms after discussing with them the short-term (up to 5 years) and longer-term benefits and risks. Offer a choice of preparations as follows:
- oestrogen and progestogen to women with a uterus
- oestrogen alone to women without a uterus
- Do not routinely offer selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs) or clonidine as first-line treatment for vasomotor symptoms alone
- Explain to women that there is some evidence that isoflavones or black cohosh may relieve vasomotor symptoms. However, explain that:
- multiple preparations are available and their safety is uncertain
- different preparations may vary
- interactions with other medicines have been reported.
Psychological Symptoms
- Consider HRT to alleviate low mood that arises as a result of the menopause
- Consider CBT to alleviate low mood or anxiety that arise as a result of the menopause
- Ensure that menopausal women and healthcare professionals involved in their care understand that there is no clear evidence for SSRIs or SNRIs to ease low mood in menopausal women who have not been diagnosed with depression (see the NICE guideline on depression in adults).
Altered Sexual Function
- Consider testosterone* supplementation for menopausal women with low sexual desire if HRT alone is not effective.
Urogenital Atrophy
- Offer vaginal oestrogen to women with urogenital atrophy (including those on systemic HRT) and continue treatment for as long as needed to relieve symptoms
- Consider vaginal oestrogen for women with urogenital atrophy in whom systemic HRT is contraindicated, after seeking advice from a healthcare professional with expertise in menopause
- If vaginal oestrogen does not relieve symptoms of urogenital atrophy, consider increasing the dose after seeking advice from a healthcare professional with expertise in menopause
- Explain to women with urogenital atrophy that:
- symptoms often come back when treatment is stopped
- adverse effects from vaginal oestrogen are very rare
- they should report unscheduled vaginal bleeding to their GP
- Advise women with vaginal dryness that moisturisers and lubricants can be used alone or in addition to vaginal oestrogen
- Do not offer routine monitoring of endometrial thickness during treatment for urogenital atrophy.
Complementary Therapies and Unregulated Preparations
- Explain to women that the efficacy and safety of unregulated compounded bioidentical hormones are unknown
- Explain to women who wish to try complementary therapies that the quality, purity and constituents of products may be unknown
- Advise women with a history of, or at high risk of, breast cancer that, although there is some evidence that St John's wort may be of benefit in the relief of vasomotor symptoms, there is uncertainty about:
- appropriate doses
- persistence of effect
- variation in the nature and potency of preparations
- potential serious interactions with other drugs (including tamoxifen, anticoagulants and anticonvulsants).
Review and Referral
- Discuss with women the importance of keeping up to date with nationally recommended health screening
- Review each treatment for short-term menopausal symptoms:
- at 3 months to assess efficacy and tolerability
- annually thereafter unless there are clinical indications for an earlier review (such as treatment ineffectiveness, side-effects or adverse events)
- Refer women to a healthcare professional with expertise in menopause if treatments do not improve their menopausal symptoms or they have ongoing troublesome side-effects
- Consider referring women to a healthcare professional with expertise in menopause if:
- they have menopausal symptoms and contraindications to HRT or
- there is uncertainty about the most suitable treatment options for their menopausal symptoms.
Starting and Stopping HRT
- Explain to women with a uterus that unscheduled vaginal bleeding is a common side effect of HRT within the first 3 months of treatment but should be reported at the 3-month review appointment, or promptly if it occurs after the first 3 months (see recommendations on endometrial cancer in the NICE guideline on suspected cancer)
- Offer women who are stopping HRT a choice of gradually reducing or immediately stopping treatment
- Explain to women that:
- gradually reducing HRT may limit recurrence of symptoms in the short term
- gradually reducing or immediately stopping HRT makes no difference to their symptoms in the longer term.
Women with, or at High Risk of, Breast Cancer
- For advice on the treatment of menopausal symptoms in women with breast cancer or at high risk of breast cancer, see the NICE guideline on early and locally advanced breast cancer and the NICE guideline on familial breast cancer
- Offer menopausal women with, or at high risk of, breast cancer:
- information on all available treatment options
- information that the SSRIs paroxetine and fluoxetine should not be offered to women with breast cancer who are taking tamoxifen
- referral to a healthcare professional with expertise in menopause.
Long-term Benefits and Risks of Hormone Replacement Therapy
Venous Thromboembolism
- Explain to women that:
- the risk of venous thromboembolism (VTE) is increased by oral HRT compared with baseline population risk
- the risk of VTE associated with HRT is greater for oral than transdermal preparations
- the risk associated with transdermal HRT given at standard therapeutic doses is no greater than baseline population risk
- Consider transdermal rather than oral HRT for menopausal women who are at increased risk of VTE, including those with a BMI over 30 kg/m2
- Consider referring menopausal women at high risk of VTE (for example, those with a strong family history of VTE or a hereditary thrombophilia) to a haematologist for assessment before considering HRT.
Cardiovascular Disease
- Ensure that menopausal women and healthcare professionals involved in their care understand that HRT:
- does not increase cardio vascular disease risk when started in women aged under 60 years
- does not affect the risk of dying from cardio vascular disease
- Be aware that the presence of cardio vascular risk factors is not a contraindication to HRT as long as they are optimally managed
- Explain to women that:
- the baseline risk of coronary heart disease and stroke for women around menopausal age varies from one woman to another according to the presence of cardio vascular risk factors
- HRT with oestrogen alone is associated with no, or reduced, risk of coronary heart disease
- HRT with oestrogen and progestogen is associated with little or no increase in the risk of coronary heart disease
- Explain to women that taking oral (but not transdermal) oestrogen is associated with a small increase in the risk of stroke. Also explain that the baseline population risk of stroke in women aged under 60 years is very low.
Type 2 Diabetes
- Explain to women that taking HRT (either orally or transdermally) is not associated with an increased risk of developing type 2 diabetes
- Ensure that women with type 2 diabetes and all healthcare professionals involved in their care are aware that HRT is not generally associated with an adverse effect on blood glucose control
- Consider HRT for menopausal symptoms in women with type 2 diabetes after taking comorbidities into account and seeking specialist advice if needed.
Breast Cancer
- Using the MHRA risk table, explain to women around the age of natural menopause that:
- the baseline risk of breast cancer for women around menopausal age varies from one woman to another according to the presence of underlying risk factors
- HRT with oestrogen alone is associated with little or no change in the risk of breast cancer
- HRT with oestrogen and progestogen can be associated with an increase in the risk of breast cancer
- any increase in the risk of breast cancer is related to treatment duration and reduces after stopping HRT.
Osteoporosis
- Give women advice on bone health and discuss these issues at review appointments (see the NICE guideline on osteoporosis: assessing the risk of fragility fracture)
- Explain to women that the baseline population risk of fragility fracture for women around menopausal age in the UK is low and varies from one woman to another
- Explain to women that their risk of fragility fracture is decreased while taking HRT and that this benefit:
- is maintained during treatment but decreases once treatment stops
- may continue for longer in women who take HRT for longer.
Dementia
- Explain to menopausal women that the likelihood of HRT affecting their risk of dementia is unknown.
Loss of Muscle Mass and Strength
- Explain to women that:
- there is limited evidence suggesting that HRT may improve muscle mass and strength
- muscle mass and strength is maintained through, and is important for, activities of daily.
Footnote
* At the time of publication (November 2015), testosterone did not have a UK marketing authorisation for this indication in women. The prescriber should follow relevant professional guidance, taking full responsibility for the decision. Informed consent should be obtained and documented. See the General Medical Council's Prescribing guidance: prescribing unlicensed medicines for further information.

