Overview
The aim of this Guidelines summary is to provide a simple, effective, economical, and empirical approach to the diagnosis of urinary tract infections (UTIs) and minimise the emergence of antibiotic resistance in the community.
The quick reference tool has been produced in consultation with general practitioners, nurses, specialists, and patient representatives.
The tool is in agreement with other publications, including NICE Clinical Knowledge Summaries (CKS) and Scottish Intercollegiate Guidelines Network (SIGN).
NICE has endorsed that this quick reference tool accurately reflects recommendations in the NICE guideline on antimicrobial stewardship and urinary tract infections.
The quick reference tool is fully referenced and graded.
The quick reference tool is not all-encompassing, as it is meant to be ‘quick reference’. Clinicians should ultimately rely on their clinical judgement and use with other recommended resources. If more detail is required, referral to the websites and references cited is suggested.
All Patients
- For all patients, please refer to the information and reference tables in joint NICE/PHE guidance: NICE guidelines on UTI (lower): antimicrobial prescribing or NICE guidelines on Pyelonephritis (acute): antimicrobial prescribing.
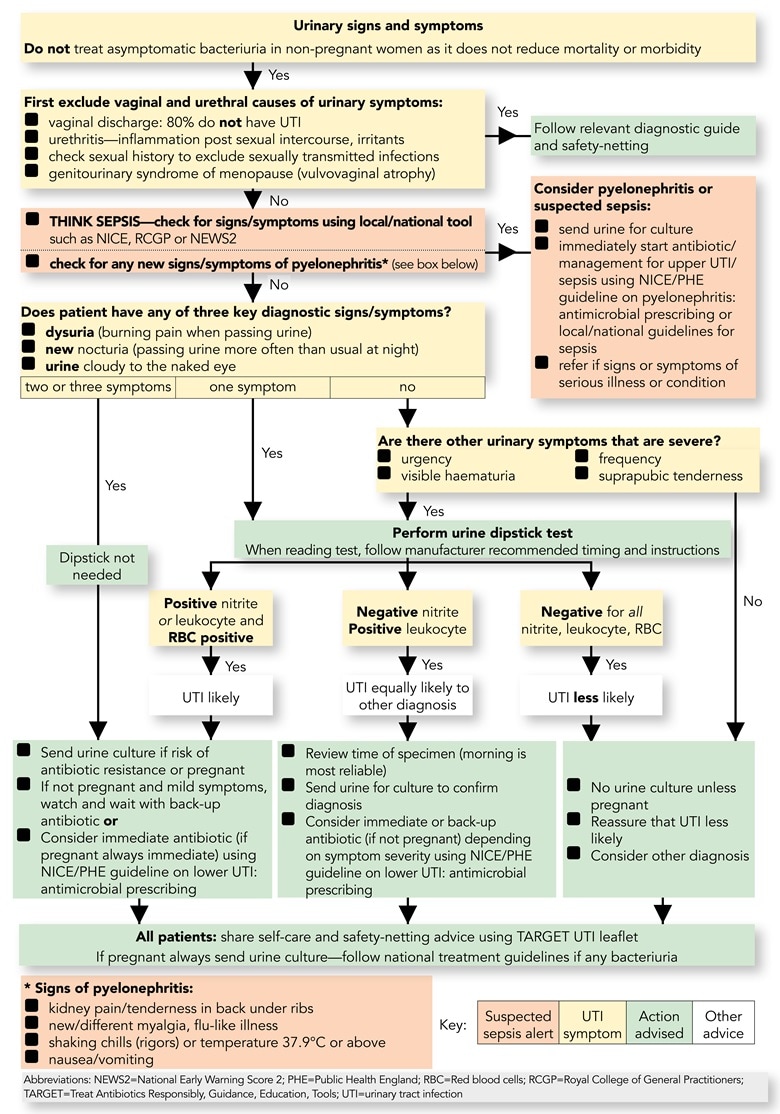
Algorithm 1: Flowchart for Women (Under 65 Years) with Suspected UTI
- Excludes women with recurrent UTI (two episodes in last 6 months, or three episodes in last 12 months) or urinary catheter.
| Guidelines summaries of NICE/PHE antimicrobial prescribing guidance are available: |
Diagnostic Points for Men Under 65 Years
- Asymptomatic bacteriuria is rare in men <65 years.
Consider Other Genitourinary Causes of Urinary Symptoms
- If sexually active, check sexual history for sexually transmitted infections (STIs), for example chlamydia and gonorrhoea
- Urethritis due to urethral inflammation post-sexual intercourse, irritants, or STIs.
Check for Pyelonephritis, Prostatitis, Systemic Infection, or Suspected Sepsis Using Local Policy
- Urinary symptoms with fever or systemic symptoms in men are strongly suggestive of prostatic involvement or pyelonephritis
- Acute prostatitis may present with feverish illness of sudden onset, symptoms of prostatitis (low back, suprapubic, perineal, or sometimes rectal pain), symptoms of UTI (dysuria, frequency, urgency or retention), or exquisitely tender prostate on rectal examination
- Recurrent or relapsing UTI in men should prompt referral to urology for investigation.
Diagnostic Points in Men
- To confirm diagnosis, always send a mid-stream urine sample for culture, collected before antibiotics are given
- Do not use urine dipsticks to rule out infection as they are unreliable for this
- A urine dipstick test with positive nitrites makes UTI more likely in men (PPV 96%). Negative for both nitrite and leucocyte makes UTI less likely, especially if symptoms are mild
- If suspected UTI, offer immediate treatment according to NICE/PHE guideline on lower UTI: antimicrobial prescribing and review choice of antibiotic with pre-treatment culture results.
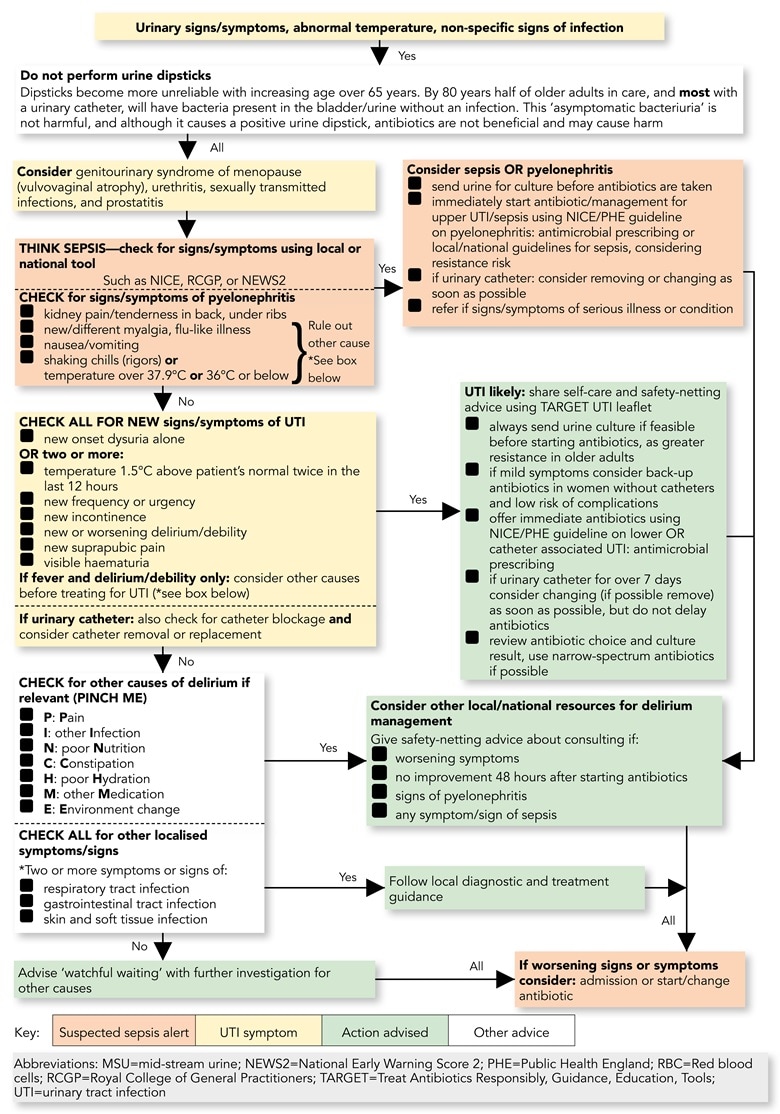
Algorithm 2: Flowchart for Suspected UTI in Catheterised Adults or Those Over 65 Years
Guidelines summaries of NICE/PHE antimicrobial prescribing guidance are available: |
Sending Urine for Culture and Interpreting Results in All Adults
|
Sampling in All Men and Women
|
How Do I Interpret a Urine Culture Result if I Suspect a UTI?
Please refer to joint NICE/PHE guidance: NICE/PHE guidelines on UTI (lower): antimicrobial prescribing or NICE/PHE guidelines on pyelonephritis (acute): antimicrobial prescribing or NICE/PHE guideline on catheter-associated UTI: antimicrobial prescribing. |
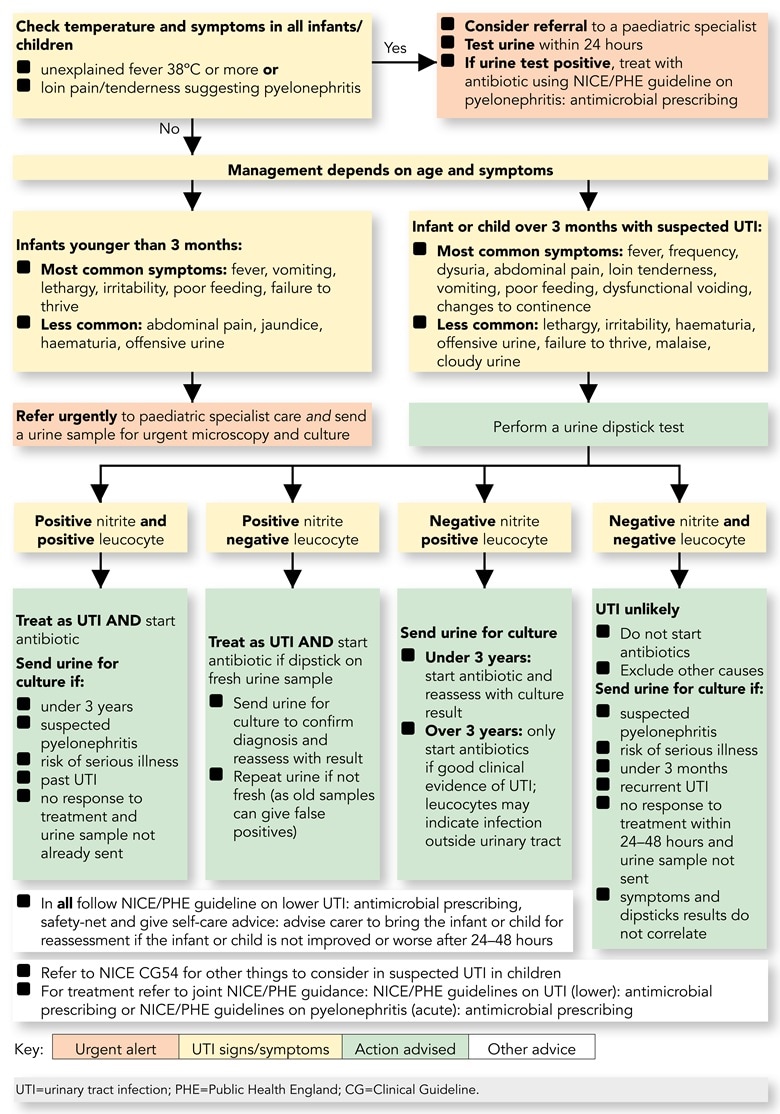
Algorithm 3: Flowchart for Infants/Children Under 16 years with Suspected UTI
- Consider UTI in any sick child and every young child with unexplained fever.
Guidelines summaries of NICE/PHE antimicrobial prescribing guidance are available: |
Key Points for Infants/Children Under 16 Years with Suspected UTI
Sampling in Children:
- If sending a urine culture, obtain sample before starting antibiotics
- If child has alternative site of infection do not test urine unless remains unwell—then test within 24 hours
- In infants/toddlers, clean catch urine advised; gentle suprapubic cutaneous stimulation using gauze soaked in cold fluid helps trigger voiding; clean catch urine using potties cleaned in hot water with washing up liquid; nappy pads cause more contamination, and parents find bags more distressing
- If non-invasive not possible consider: catheter sample, or suprapubic aspirate (with ultrasound guidance)
- Culture urine within 4 hours of collection, if this is not possible refrigerate, or use boric acid preservative. Boric acid can cause false negative culture if urine not filled to correct mark on specimen bottle.
Interpretation of Culture Results in Children:
- Single organism ≥106 cfu/l (103 cfu/ml) may indicate UTI in voided urine
- Any growth from a suprapubic aspirate is significant
- Pyuria ≥107 WBC/l (104 WBC/ml) usually indicate UTI, especially with clinical symptoms but may be absent.
Other Diagnostic Tests
- Do not use CRP to differentiate upper UTI from lower UTI.
Ultrasound
- If proven UTI is atypical (seriously ill, poor urine flow, abdominal or bladder mass, raised creatinine, septicaemia, failure to respond to antibiotic within 48 hours, non-E.coli infection): ultrasound all children in acute phase and undertake renal imaging within 4–6 months if under 3 years
- All ages with recurrent UTI
- For children under 6 months or those with non-E.coli UTI: ultrasound within 6 weeks if UTI not atypical and responding to antibiotics
- Refer to NICE CG54 for other things to consider in suspected UTI in children.

