Overview
This Guidelines summary combines recommendations from the UK Sepsis Trust to give recommendations on the recognition and management of sepsis in adults, children, and young people over 12 years of age. The recommendations in this summary are applicable to primary care settings.
Sepsis Definitions
Sepsis is characterised by a dysregulated host response to infection mediated by the immune system and resulting in organ dysfunction, potentially multi-organ failure, shock, and death.
Septic shock is defined as a subset of sepsis where particularly profound circulatory, cellular, and metabolic abnormalities substantially increase mortality.
Determining in whom to Consider Sepsis/Record Physiological Parameters
A ‘typical’ GP will see one, maybe two, cases of sepsis per year among many thousands of patients with self-limiting or minor infection. No recognition pathway is a substitute for clinical acumen. NICE NG51 recommends that health professionals think ‘could this be sepsis?’ if a person presents with signs or symptoms that indicate possible infection.
At-risk Groups
In patients who have one or more of the following risk factors, the clinician should give particular consideration as to whether face-to-face assessment (as opposed to telephone consultation) in the context of a potential infection is appropriate:
- Age >75 years
- Impaired immunity (for example, diabetes, steroids, chemotherapy)
- Recent trauma/surgery/invasive procedure
- Indwelling lines/IVDU/broken skin.
Sepsis Risk Stratification
- Patients in whom sepsis is considered should have a full set of physiological observations taken to include temperature, heart rate, respiratory rate, blood pressure, and level of consciousness. Where resources permit, the measurement of oxygen saturations using a pulse oximeter should be performed in addition to basic physiological assessment
- It is not always possible to define a source of infection in a patient presumed to have sepsis, particularly at initial assessment. It is important to reinforce that patients with signs and symptoms of infection together with physiological deterioration in the absence of a clear source should continue to be presumed to have sepsis.
Algorithm 1: Screening and Action Tool for Adults and Children and Young People 12 Years and Over—General Practice
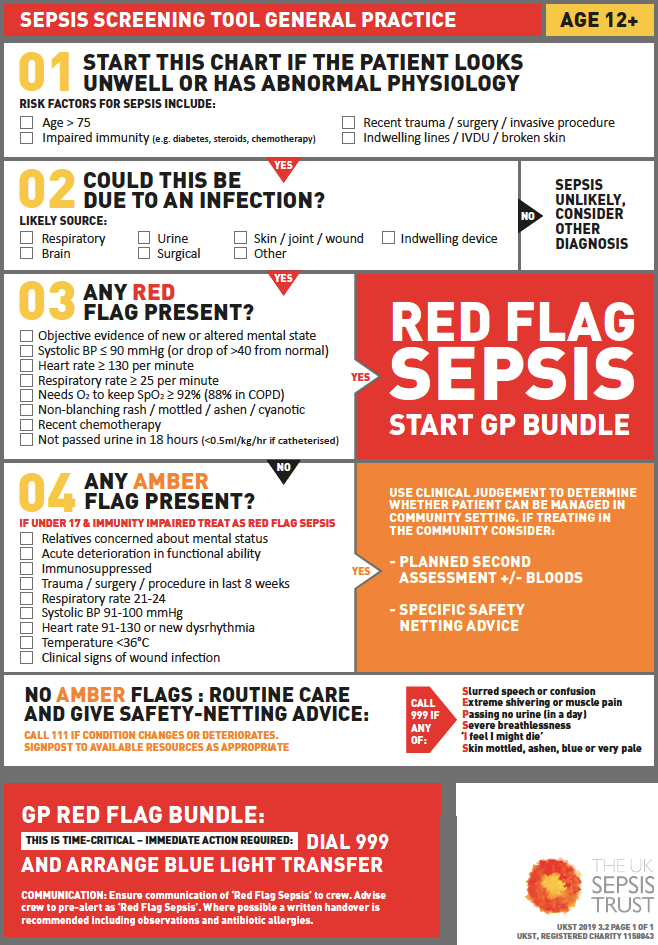
Confirming that Sepsis Risk Stratification is Required
- In the context of presumed infection, are any of the following true (common sources: chest, urinary tract infection [UTI], abdominal organs):
- patient looks very unwell
- family or carer is very concerned
- there is ongoing deterioration
- physiology is abnormal for this patient
- The first step in sepsis risk stratification should be to confirm or exclude the presence of any ONE high risk, Red Flag Sepsis criterion.
Red Flag Sepsis (See Algorithm 1)
- Any patient with presumed sepsis who has one or more Red Flag Sepsis criteria should be assumed to have sepsis or septic shock, and immediately transferred to hospital if appropriate. Patients who have no Red Flag Sepsis criteria should immediately be screened for Amber Flag Sepsis.
Amber Flag Sepsis
- For patients 18 years and over, NICE recommends that the presence of any one amber flag criterion prompt a binary clinical decision. Clinical judgement should be used to determine whether the patient can be managed in the community setting or requires hospital assessment. For those in whom community-based care is deemed safe and appropriate, consideration should be given to providing a scheduled review appointment, and a clear record should be made of the decision, rationale, and any safety netting provided
- Written and verbal safety netting is essential for patients with Amber Flag Sepsis deemed appropriate to remain in the community (see Section 8 of the full guideline)
- If a patient with one or more amber flags is aged 17 years or younger and is immunocompromised, they should be treated as Red Flag Sepsis and immediate transfer for hospital assessment arranged
- Some practices have begun to explore the use of the National Early Warning Score (NEWS, Algorithm 2) in higher risk groups to identify and communicate potential for deterioration.
Algorithm 2: NEWS2 Observation Chart
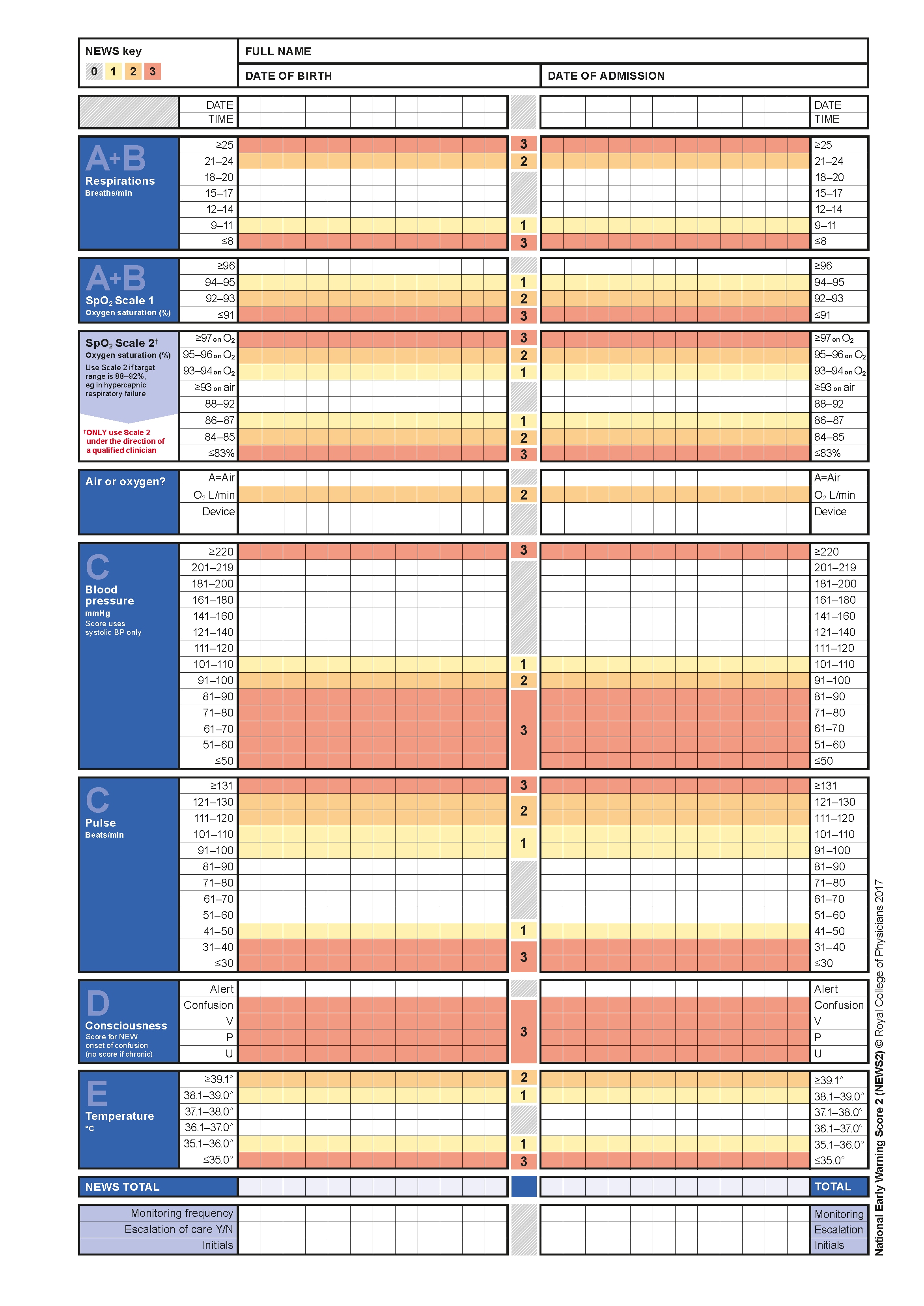
NEWS=National Early Warning Score; SpO2=oxygen saturation; BP=blood pressure.
Recommendations for Safety Netting
If the patient is not to be referred for hospital assessment, there must be adequate written and verbal safety netting. Any safety netting advice given should be clearly documented in the patient’s notes, together with observations and antimicrobial therapy offered. It is good practice to agree a planned next-day review assessment in any patient with Amber Flag Sepsis managed in the community, together with an invitation for open self-referral should the patient deteriorate or they or their relatives be concerned.
Communication with Ambulance Service and Secondary Care
- For patients identified with Red Flag Sepsis, immediate arrangement should be made for urgent transfer for hospital assessment. This should be by ‘blue light’ ambulance, with a Paramedic crew if immediately available. The call should include direct reference to the acuity of the condition, using the term ‘Red Flag Sepsis’. If the call is made in the presence of the patient or their relatives, it may be preferable to state that the patient has suspected sepsis and give observations (such as using the NEWS score)
- Where there are one or more Amber Flags in the absence of any Red Flag, clinical judgement will determine appropriate action
- Patients with sepsis can deteriorate rapidly
- The urgency of hospital transfer is not as clear-cut as with Red Flag Sepsis, and clinical judgement will inform disposition. The call to the Ambulance Service should include direct reference to the acuity of the condition, using the term ‘Amber Flag Sepsis’.
Early Care Options for Patients with Sepsis
Early Care Options for Patients with Sepsis (Red Flag Sepsis and Amber Flags Where Decision is Made to Refer for Hospital Assessment)
- The key immediate interventions that increase survival are described in a bundle termed the Sepsis Six (Algorithm 3). This bundle has been shown to be associated with significant mortality reductions when applied within the first hour.
Algorithm 3: The Sepsis Six
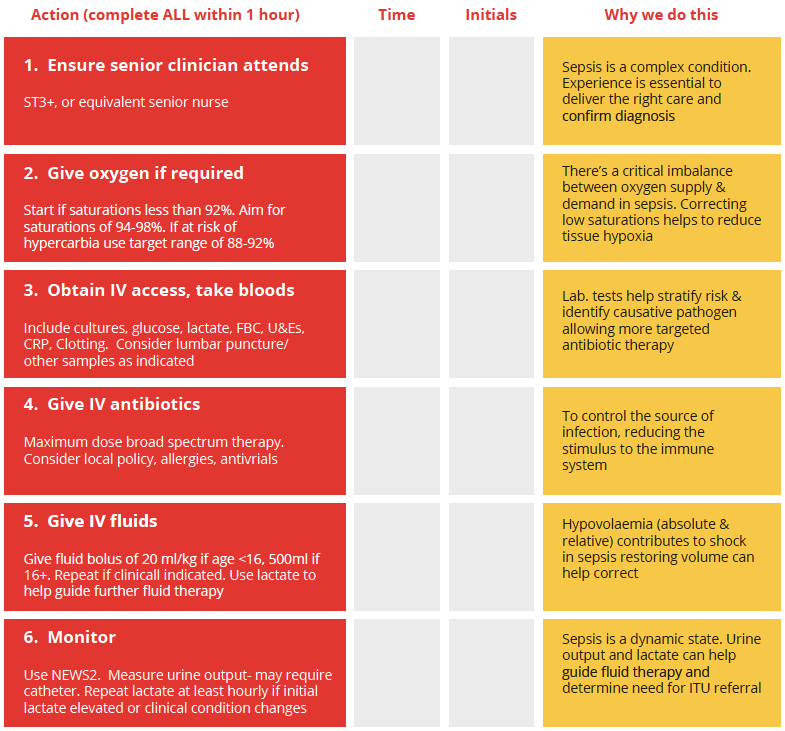
ST3+=specialty trainees 3+; FBC=full blood count; U&Es=urea and electrolytes; CRP=C-reactive protein; NEWS2=National Early Warning Score 2; ITU=intensive therapy unit.
- The key immediate interventions that increase survival are described in a bundle termed the Sepsis Six (see Algorithm 3). This bundle has been shown to be associated with significant mortality reductions when applied within the first hour
- While few GPs will have the resources to provide the entirety of this bundle of care, it is included to illustrate the time-critical nature of Red Flag Sepsis and the need for collaborative care pathways
- Where resources permit, GPs should initiate oxygen therapy to maintain target saturations of 94% or higher
- where patients are known to have moderate to severe pulmonary disease (and where available), the UK Sepsis Trust still recommends that oxygen be administered but to maintain a lower target oxygen saturations above 88%
- Particularly in remote areas, consideration should be given to the delivery of other elements of the Sepsis Six
- For further information on advanced care for patients with sepsis, refer to section 6 of the full guideline.

