Latest Guidance UpdatesAugust 2023: NICE reviewed the evidence on the use of Wells score and D-dimer in the diagnostic pathways for pulmonary embolism and deep vein thrombosis in people with COVID-19, and updated recommendations. NICE also refreshed the wording of its recommendation on people with a negative proximal leg vein ultrasound scan and a positive D-dimer test result. |
Overview
This Guidelines summary covers diagnosis and initial management, outpatient treatment for low-risk pulmonary embolism (PE), anticoagulation treatment for suspected or confirmed deep vein thrombosis (DVT) or PE, and information and support for people having anticoagulation treatment.
This summary only covers key recommendations for primary care. Refer to the full guideline for a complete set of recommendations.
Reflecting on your Learnings
Reflection is important for continuous learning and development, and a critical part of the revalidation process for UK healthcare professionals. Click here to access the Guidelines Reflection Record.
Diagnosis and Initial Management
Signs or Symptoms of DVT
- For people who present with signs or symptoms of DVT, such as a swollen or painful leg, assess their general medical history and do a physical examination to exclude other causes.
- If DVT is suspected, use the 2-level DVT Wells score (Table 1) to estimate the clinical probability of DVT.
Algorithm 1: Suspected DVT: Diagnosis and Initial Management
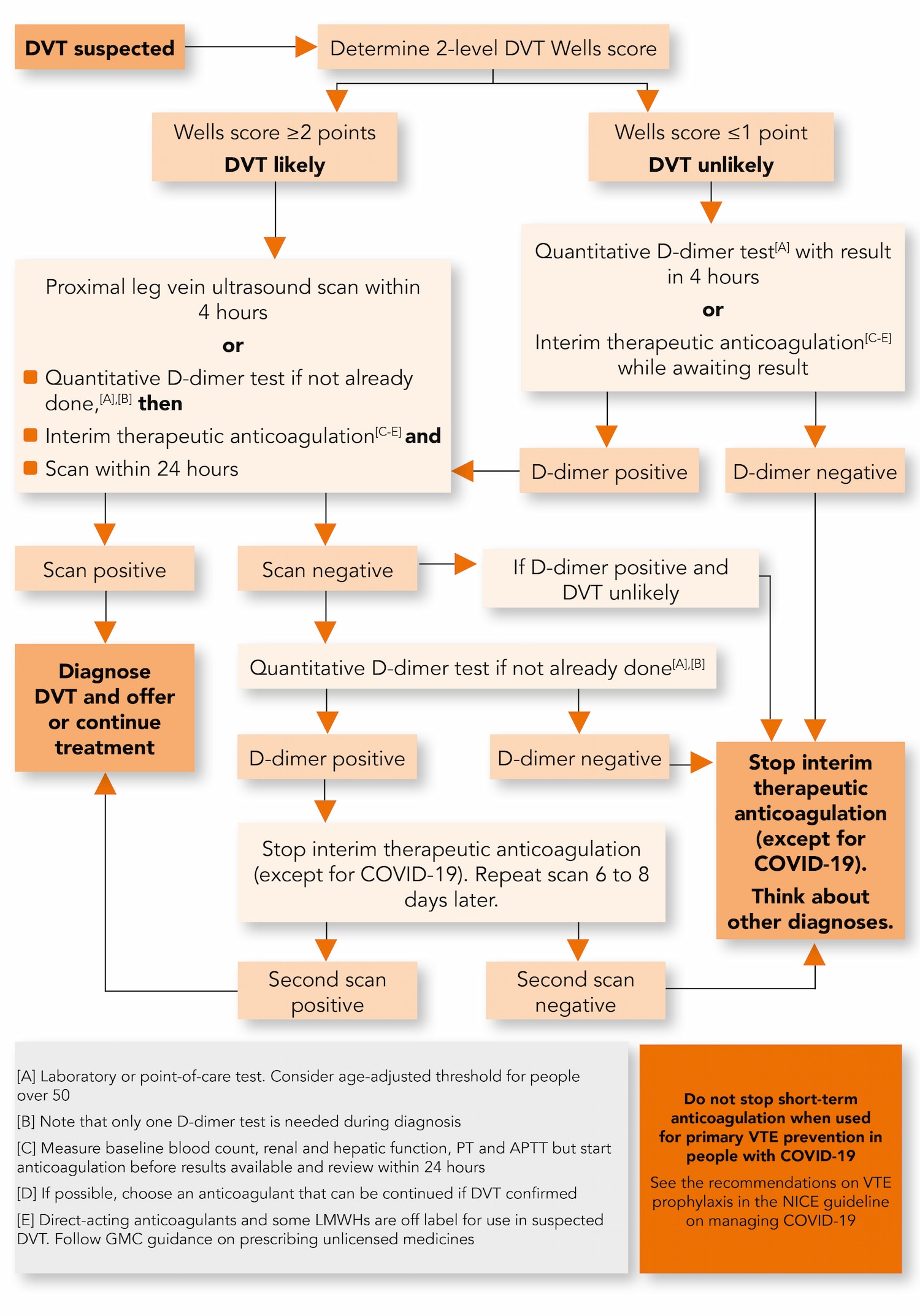
Table 1: Two-level DVT Wells Score
| Clinical Feature | Points |
|---|---|
| Active cancer (treatment ongoing, within 6 months, or palliative) | 1 |
| Paralysis, paresis or recent plaster immobilisation of the lower extremities | 1 |
| Recently bedridden for 3 days or more, or major surgery within 12 weeks requiring general or regional anaesthesia | 1 |
| Localised tenderness along the distribution of the deep venous system | 1 |
| Entire leg swollen | 1 |
| Calf swelling at least 3 cm larger than asymptomatic side | 1 |
| Pitting oedema confined to the symptomatic leg | 1 |
| Collateral superficial veins (non-varicose) | 1 |
| Previously documented DVT | 1 |
| An alternative diagnosis is at least as likely as DVT | -2 |
| Clinical Probability Simplified Scores | |
| DVT likely | 2 points or more |
| DVT unlikely | 1 point or less |
| Adapted with permission from Wells et al. (2003) Evaluation of D-dimer in the diagnosis of suspected deep-vein thrombosis | |
DVT Likely (Wells Score 2 Points or More)
- Offer people with a likely DVT Wells score (2 points or more):
- a proximal leg vein ultrasound scan, with the result available within 4 hours if possible (if the scan result cannot be obtained within 4 hours follow the following recommendation)
- a D-dimer test if the scan result is negative.
- If a proximal leg vein ultrasound scan result cannot be obtained within 4 hours, offer people with a DVT Wells score of 2 points or more:
- a D-dimer test, then
- interim therapeutic anticoagulation (see the section on interim therapeutic anticoagulation for suspected DVT or PE) and
- a proximal leg vein ultrasound scan with the result available within 24 hours.
- For people with a positive proximal leg vein ultrasound scan:
- offer or continue anticoagulation treatment (see the section on anticoagulation treatment for confirmed DVT or PE) or
- if anticoagulation treatment is contraindicated, offer a mechanical intervention (see the section on mechanical interventions in this summary and the full guideline).
For people with symptomatic iliofemoral DVT, see the section on thrombolytic therapy in the full guideline.
- For people with a negative proximal leg vein ultrasound scan and a positive D-dimer test result:
- stop interim therapeutic anticoagulation, but do not stop:
- long-term anticoagulation when used for secondary prevention, or
- short-term anticoagulation when used for primary venous thromboembolism (VTE) prevention in people with COVID-19 (see the recommendations on VTE prophylaxis in the NICE guideline on managing COVID-19)
- offer a repeat proximal leg vein ultrasound scan 6 to 8 days later and
- if the repeat scan result is positive, follow the actions in the previous recommendation
- if the repeat scan result is negative, follow the actions in the following recommendation
- stop interim therapeutic anticoagulation, but do not stop:
- For people with a negative proximal leg vein ultrasound scan and a negative D-dimer test result:
- stop interim therapeutic anticoagulation, but do not stop:
- long-term anticoagulation when used for secondary prevention, or
- short-term anticoagulation when used for primary VTE prevention in people with COVID-19 (see the recommendations on VTE prophylaxis in the NICE guideline on managing COVID-19)
- stop interim therapeutic anticoagulation, but do not stop:
- think about alternative diagnoses
- tell the person that it is not likely they have DVT. Discuss with them the signs and symptoms of DVT and when and where to seek further medical help.
DVT Unlikely (Wells Score 1 Point or Less)
- Offer people with an unlikely DVT Wells score (1 point or less):
- a D-dimer test with the result available within 4 hours (see the secion on D-dimer testing) or
- if the D-dimer test result cannot be obtained within 4 hours, offer interim therapeutic anticoagulation while awaiting the result (see the section on interim therapeutic anticoagulation for suspected DVT or PE).
- If the D-dimer test result is negative, follow the actions in the above recommendation on people with a negative proximal leg vein ultrasound and a negative D-dimer test result.
- If the D-dimer test result is positive, offer:
- a proximal leg vein ultrasound scan, with the result available within 4 hours if possible or
- interim therapeutic anticoagulation (see the section on interim therapeutic anticoagulation for suspected DVT or PE) and a proximal leg vein ultrasound scan with the result available within 24 hours.
- If the proximal leg vein ultrasound scan is:
- positive, follow the actions in the above recommendation on people with a positive proximal leg vein ultrasound scan
- negative, follow the actions in the above recommendation on people with a negative proximal leg vein ultrasound scan and a negative D-dimer test result, that is:
- stop interim therapeutic anticoagulation, but do not stop:
- long-term anticoagulation when used for secondary prevention, or
- short-term anticoagulation when used for primary VTE prevention in people with COVID-19 (see the recommendations on VTE prophylaxis in the NICE guideline on managing COVID-19)
- think about alternative diagnoses
- tell the person that it is not likely they have DVT. Discuss with them the signs and symptoms of DVT and when and where to seek further medical help.
- stop interim therapeutic anticoagulation, but do not stop:
D-dimer Testing
- When offering D-dimer testing for suspected DVT or PE, consider a point-of-care test if laboratory facilities are not immediately available.
- If using a point-of-care D-dimer test, choose a fully quantitative test.
- When using a point-of-care or laboratory D-dimer test, consider an age-adjusted D-dimer test threshold for people aged over 50.
Signs or Symptoms of PE
- For people who present with signs or symptoms of PE, such as chest pain, shortness of breath or coughing up blood, assess their general medical history, do a physical examination and offer a chest X-ray to exclude other causes.
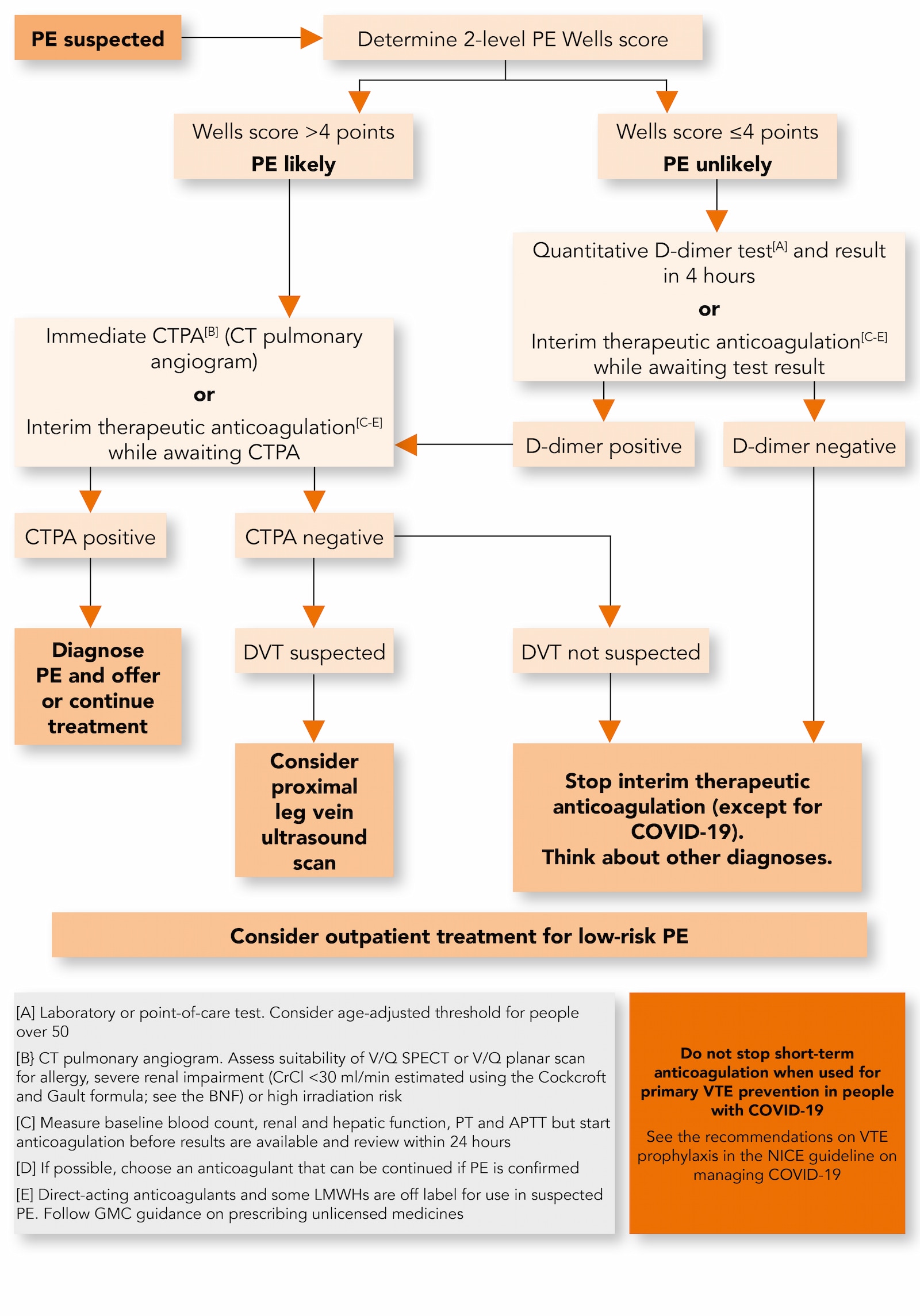
Algorithm 2: Suspected PE: Diagnosis and Initial Management
Pulmonary Embolism Rule-out Criteria (The PERC Rule)
- If clinical suspicion of PE is low based on the overall clinical impression (from general medical history, physical examination and any initial investigations such as electrocardiography or chest X-ray), and other diagnoses are feasible, consider using the pulmonary embolism rule-out criteria (PERC) to help determine whether any further investigations for PE are needed. Be aware that the PERC rule has not been validated in people with COVID-19.
- If PE is suspected, use the 2-level PE Wells score (Table 2) to estimate the clinical probability of PE.
Table 2: Two-level PE Wells Score
| Clinical Feature | Points |
|---|---|
| Clinical signs and symptoms of DVT (minimum of leg swelling and pain with palpation of the deep veins) | 3 |
| An alternative diagnosis is less likely than PE | 3 |
| Heart rate more than 100 beats per minute | 1.5 |
| Immobilisation for more than 3 days or surgery in the previous 4 weeks | 1.5 |
| Previous DVT/PE | 1.5 |
| Haemoptysis | 1 |
| Malignancy (on treatment, treated in the last 6 months, or palliative) | 1 |
| Clinical Probability Simplified Scores | Points |
| PE likely | More than 4 points |
| PE unlikely | 4 points or less |
| Adapted with permission from Wells et al. (2000) Derivation of a simple clinical model to categorize patients’ probability of pulmonary embolism: increasing the model’s utility with the SimpliRED D-dimer | |
PE Likely (Wells Score More Than 4 Points)
- For people with a likely PE Wells score (more than 4 points):
- offer a computed tomography pulmonary angiogram (CTPA) immediately if possible or
- for people with an allergy to contrast media, severe renal impairment (estimated creatinine clearance[A] less than 30 ml/min) or a high risk from irradiation, assess the suitability of a ventilation/perfusion single photon emission computed tomography (V/Q SPECT) scan or, if a V/Q SPECT scan is not available, a V/Q planar scan, as an alternative to CTPA.
If a CTPA, V/Q SPECT or V/Q planar scan cannot be done immediately, offer interim therapeutic anticoagulation (see the section on interim therapeutic anticoagulation for suspected DVT or PE).
- If PE is identified by CTPA, V/Q SPECT or V/Q planar scan:
- offer or continue anticoagulation treatment (see the section on anticoagulation treatment for confirmed DVT or PE) or
- if anticoagulation treatment is contraindicated, consider a mechanical intervention (see the section on mechanical interventions in this summary and the full guideline).
For people with PE and haemodynamic instability see the section on thrombolytic therapy in the full guideline.
- If PE is not identified by CTPA, V/Q SPECT or V/Q planar scan:
- consider a proximal leg vein ultrasound scan if DVT is suspected
- if DVT is not suspected:
- stop interim therapeutic anticoagulation, but do not stop:
- long-term anticoagulation when used for secondary prevention, or
- short-term anticoagulation when used for primary VTE prevention in people with COVID-19 (see the recommendations on VTE prophylaxis in the NICE guideline on managing COVID-19)
- think about alternative diagnoses
- tell the person that it is not likely they have PE. Discuss with them the signs and symptoms of PE and when and where to seek further medical help.
- stop interim therapeutic anticoagulation, but do not stop:
PE Unlikely (Wells Score 4 Points or Less)
- Offer people with an unlikely PE Wells score (4 points or less):
- a D-dimer test with the result available within 4 hours if possible (see the section on D-dimer testing) or
- if the D-dimer test result cannot be obtained within 4 hours (in any setting), offer interim therapeutic anticoagulation while awaiting the result (see the section on interim therapeutic anticoagulation for suspected DVT or PE).
- If the D-dimer test result is:
- positive, follow the actions in the recommendation on people with a likely PE Wells score (more than 4 points) and PE that is identified by CTPA, V/Q SPECT or V/Q planar scan
- negative:
- stop interim therapeutic anticoagulation, but do not stop:
- long-term anticoagulation when used for secondary prevention, or
- short-term anticoagulation when used for primary VTE prevention in people with COVID-19 (see the recommendations on VTE prophylaxis in the NICE guideline on managing COVID-19)
- stop interim therapeutic anticoagulation, but do not stop:
- think about alternative diagnoses
- tell the person that it is not likely they have PE. Discuss with them the signs and symptoms of PE and when and where to seek further medical help.
Signs or Symptoms of Both DVT and PE
- For people who present with signs or symptoms of both DVT and PE, carry out initial diagnostic investigations for either DVT or PE, basing the choice of diagnostic investigations on clinical judgement.
Outpatient Treatment for Low-Risk PE
- Consider outpatient treatment for suspected or confirmed low-risk PE, using a validated risk stratification tool to determine the suitability of outpatient treatment.
- When offering outpatient treatment to people with suspected PE, follow the recommendations in this guideline on diagnosis and initial management.
- When offering outpatient treatment to people with confirmed PE, follow the recommendations in the section on anticoagulation treatment for confirmed DVT or PE.
- Agree a plan for monitoring and follow-up with people having outpatient treatment for suspected or confirmed low-risk PE. Give them:
- written information on symptoms and signs to look out for, including the potential complications of thrombosis and of treatment
- direct contact details of a healthcare professional or team with expertise in thrombosis who can discuss any new symptoms or signs, or other concerns
- information about out-of-hours services they can contact when their healthcare team is not available.
Anticoagulation Treatment for Suspected or Confirmed DVT or PE
NICE has produced visual summaries of the recommendations on anticoagulation treatment for DVT or PE. See Algorithms 1 and 2.- When offering anticoagulation treatment follow the recommendations on shared decision making and supporting adherence in the NICE guidelines on medicines optimisation, medicines adherence, patient experiences in adult NHS services and shared decision making.
Interim Therapeutic Anticoagulation for Suspected DVT or PE
- Follow the recommendations on when to offer interim therapeutic anticoagulation for suspected proximal DVT or PE in the section on diagnosis and initial management.
- If possible, choose an interim anticoagulant that can be continued if DVT or PE is confirmed (see the section on anticoagulation treatment for confirmed DVT or PE).
In March 2020, direct-acting anticoagulants and some low molecular weight heparins (LMWHs) were off label for the treatment of suspected DVT or PE. See NICE's information on prescribing medicines.
- When using interim therapeutic anticoagulation for suspected proximal DVT or PE:
- carry out baseline blood tests including full blood count, renal and hepatic function, prothrombin time (PT) and activated partial thromboplastin time (APTT)
- do not wait for the results of baseline blood tests before starting anticoagulation treatment
- review, and if necessary act on, the results of baseline blood tests within 24 hours of starting interim therapeutic anticoagulation.
Anticoagulation Treatment for Confirmed DVT or PE
- Offer anticoagulation treatment for at least 3 months to people with confirmed proximal DVT or PE. For recommendations on treatment after 3 months see the section on long-term anticoagulation for secondary prevention in the full guideline.
- If not already done, carry out baseline blood tests, as outlined in the above recommendation on using interim therapeutic anticoagulation for suspected proximal DVT or PE, when starting anticoagulation treatment
- When offering anticoagulation treatment, take into account comorbidities, contraindications and the person’s preferences.
Follow the recommendations on anticoagulation treatment in the sections on:
- DVT or PE in people at extremes of body weight (in the full guideline)
- PE with haemodynamic instability (in the full guideline)
- DVT or PE with renal impairment or established renal failure
- DVT or PE with active cancer (in the full guideline)
- DVT or PE with triple positive antiphospholipid syndrome (in the full guideline).
- Offer either apixaban or rivaroxaban to people with confirmed proximal DVT or PE (but see recommendations 1.3.11 to 1.3.20 in the full guideline for people with any of the clinical features listed in the previous recommendation). If neither apixaban nor rivaroxaban is suitable offer:
- LMWH for at least 5 days followed by dabigatran or edoxaban or
- LMWH concurrently with a vitamin K antagonist (VKA) for at least 5 days, or until the international normalised ratio (INR) is at least 2.0 in 2 consecutive readings, followed by a VKA on its own.
- Do not routinely offer unfractionated heparin (UFH) with a VKA to treat confirmed proximal DVT or PE unless the person has renal impairment or established renal failure (see the recommendations on anticoagulation treatment for DVT or PE with renal impairment or established renal failure) or an increased risk of bleeding.
- Do not routinely offer self-management or self-monitoring of INR to people who have had DVT or PE and are having treatment with a VKA.
Anticoagulation Treatment for DVT or PE With Renal Impairment or Established Renal Failure
In March 2020, some LMWHs were off label for the treatment of DVT or PE in people with severe renal impairment (estimated creatinine clearance 15 ml/min to 30 ml/min) or established renal failure (estimated creatinine clearance less than 15 ml/min). See NICE's information on prescribing medicines.- Offer people with confirmed proximal DVT or PE and renal impairment (estimated creatinine clearance[A] between 15 ml/min and 50 ml/min) one of:
- apixaban
- rivaroxaban
- LMWH for at least 5 days followed by:
- edoxaban or
- dabigatran if estimated creatinine clearance is 30 ml/min or above
- LMWH or UFH, given concurrently with a VKA for at least 5 days or until the INR is at least 2.0 in 2 consecutive readings, followed by a VKA on its own.
Note the cautions and requirements for dose adjustment and monitoring in the medicine’s SPC, and follow locally agreed protocols or advice from a specialist or multidisciplinary team.
- Offer people with confirmed proximal DVT or PE and established renal failure (estimated creatinine clearance[A] less than 15 ml/min) one of:
- LMWH
- UFH
- LMWH or UFH concurrently with a VKA for at least 5 days or until the INR is at least 2.0 in 2 consecutive readings, followed by a VKA on its own.
Note the cautions and requirements for dose adjustment and monitoring in the medicine’s SPC, and follow locally agreed protocols or advice from a specialist or multidisciplinary team.
Treatment Failure
- If anticoagulation treatment fails:
- check adherence to anticoagulation treatment
- address other sources of hypercoagulability
- increase the dose of anticoagulant or change to an anticoagulant with a different mode of action.
Information and Support for People Having Anticoagulation Treatment
- Give people having anticoagulation treatment verbal and written information about:
- how to use anticoagulants
- how long to take anticoagulants
- possible side effects of anticoagulants and what to do if these occur
- how other medications, foods and alcohol can affect oral anticoagulation treatment
- any monitoring needed for their anticoagulant treatment
- how anticoagulants may affect their dental treatment
- taking anticoagulants if they are planning pregnancy or become pregnant
- how anticoagulants may affect activities such as sports and travel
- when and how to seek medical help.
- Give people who are having anticoagulation treatment information and an ‘anticoagulant alert card’ that is specific to their treatment. Advise them to carry the ‘anticoagulant alert card’ at all times.
- Be aware that heparins are of animal origin and that apixaban and rivaroxaban contain lactose from cow’s milk. For people who have concerns about using animal products because of a religious or ethical belief, or a food intolerance, see the section on giving information and planning for discharge in the NICE guideline on venous thromboembolism in over 16s.
Mechanical Interventions
For recommendations on inferior vena caval filters and percutaneous mechanical thrombectomy, refer to the full guideline.Elastic Graduated Compression Stockings
- Do not offer elastic graduated compression stockings to prevent post-thrombotic syndrome or VTE recurrence after a DVT. This recommendation does not cover the use of elastic stockings for the management of leg symptoms after DVT.
- If offering elastic graduated compression stockings to manage leg symptoms after DVT, explain how to apply and use them, how long they should be worn and when they should be replaced.
Footnote
[A] Creatinine clearance estimated using the Cockcroft and Gault formula; see the BNF’s information on prescribing in renal impairment.

