Latest Guidance Updates13 May 2022: new links and referrals to the NICE guideline on prostate cancer, updated prostate cancer patient pathway, minor wording changes, and a new recommendation added in the section, PSA Test, on discussing the test in the absence of symptoms. |
Overview
This updated prostate cancer risk management programme guidance aims to help GPs give clear and balanced information to asymptomatic men who ask about prostate-specific antigen (PSA) testing. The PSA test is available for free to any well man aged 50 years and over who requests it.
GPs should follow the NICE guideline on suspected cancer for the management of men who have symptoms of prostate disease.
Reflecting on your Learnings
Reflection is important for continuous learning and development, and a critical part of the revalidation process for UK healthcare professionals. Click here to access the Guidelines Reflection Record.
Prostate Cancer
- Factors that increase the risk of prostate cancer include:
- age—prostate cancer is rare under the age of 50 and risk increases with age
- having a close relative, for example, brother or father, who has had prostate cancer
- ethnicity—the lifetime risk is one in four for men of black ethnic origin compared to one in eight for white men
- Prostate cancer is common and may not cause any symptoms or shorten life. Some tested men may therefore face unnecessary diagnosis (overdiagnosis) of prostate cancer, as well as associated anxiety, medical tests, and treatments with side effects.
PSA Test
- The PSA test is a blood test that can help diagnose prostate problems. PSA levels can be raised in a number of conditions, such as a urinary infection, an enlarged prostate, prostatitis, or prostate cancer
- Most men will have a PSA level <3 ng/ml. About three in four men with a raised PSA level (≥3 ng/ml) will not have cancer. A small proportion of men who have a low PSA level will later be found to have prostate cancer
- Before a PSA test men should not have:
- an active urinary infection or within the previous 6 weeks
- ejaculated in the previous 48 hours
- exercised vigorously (for example, cycling), in the previous 48 hours
- had a urological intervention such as prostate biopsy in the previous 6 weeks
- When taking blood for PSA testing:
- ensure the specimen will reach the laboratory in time for the serum to be separated within 16 hours
- send samples to an International Organization for Standardization-accredited laboratory
- repeat the test if not taken in ideal circumstances
- A PSA test will not distinguish between aggressive tumours (which are at an early stage but will develop quickly) and those which are not. Further tests may provide valuable information
- In the presence of symptoms of prostate disease, GPs should refer to the Urological Cancers section in the NICE guideline on suspected cancer
- In the absence of symptoms, GPs should discuss the pros and cons of PSA tests with the patient. If a subsequent PSA test result shows raised PSA levels, the GP should use their clinical judgement to consider whether a referral is appropriate.
Algorithm 1: PSA Testing and Prostate Cancer Patient Pathway
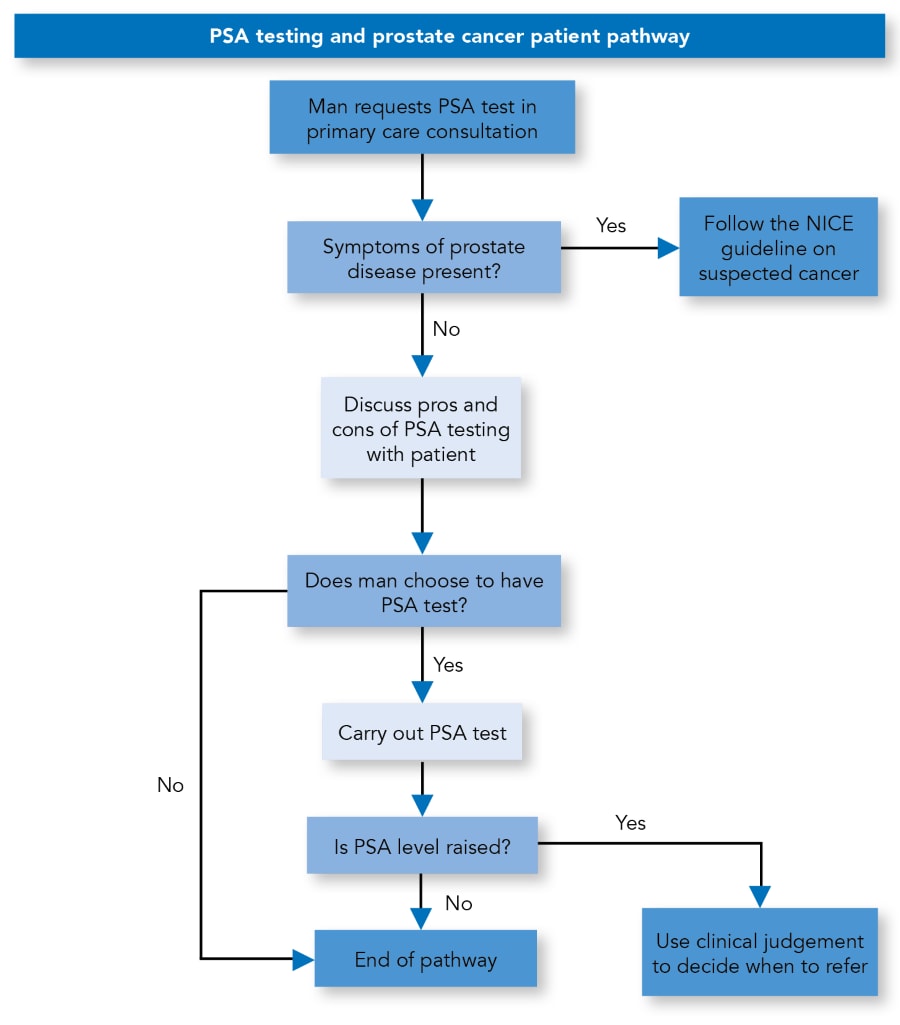
Contains public sector information licensed under the Open Government Licence v3.0.
Digital Rectal Examination
- Digital rectal examination allows assessment of the prostate for signs of prostate cancer (a hard gland, sometimes with palpable nodules) or benign enlargement (smooth, firm, enlarged gland). A gland that feels normal does not exclude a tumour
- The NICE guideline on prostate cancer suggests that the following investigations and treatments will be part of the onward diagnosis and management of your patient.
Multiparametric MRI
- Pre-biopsy multiparametric magnetic resonance imaging (mpMRI) of the prostate gland aims to accurately locate clinically significant prostate cancer and facilitate targeted biopsy. Studies suggest that by using mpMRI prostate biopsy can be avoided by more than 25% of men, and may reduce detection of clinically insignificant cancers.
Biopsy
- A biopsy may confirm the diagnosis of prostate cancer and provide useful prognostic information
- Most men experience blood in urine and semen after biopsy. About two out of five men describe biopsy as painful. The most common complications are bleeding and infections including a small risk of sepsis
- Neither mpMRI nor prostate biopsy will detect all prostate cancers.
Management and Treatment
- The NICE guideline on prostate cancer includes recommendations about the treatment and management options for localised prostate cancer. The options include one or more of:
- monitoring (surveillance)
- radical prostatectomy (open, laparoscopic, or robotically assisted laparoscopic)
- targeted and external beam radiotherapy
- brachytherapy (low and high dose rate)
- hormone therapy
- The options chosen will depend on a number of factors, including the man’s general health and the stage of disease. Surgery and radiotherapy may offer the possibility of a cure but can have significant adverse effects on a man’s quality of life and wellbeing.
Information for Well Men Aged 50 Years and Over
Algorithm 2: Infographic of the PSA Test
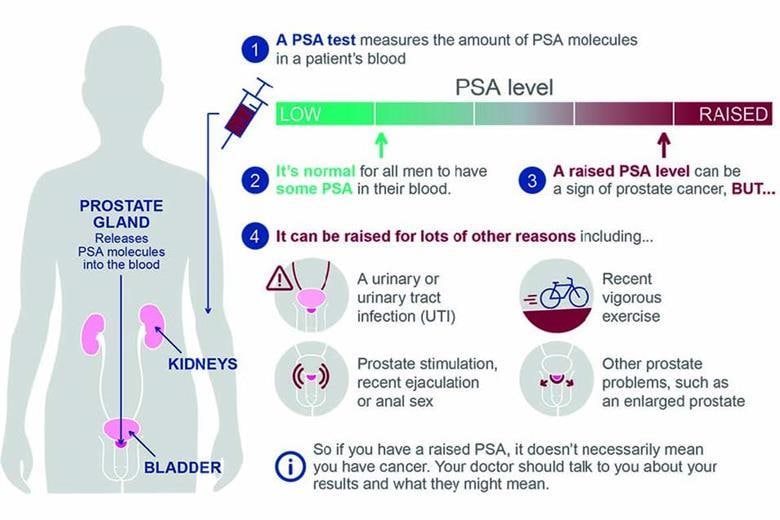
© UK Health Security Agency. Contains public sector information licensed under the Open Government Licence v3.0.
- Refer to Algorithm 2 and direct patients to the information sheet for well men aged 50 years and over for a summary of the potential benefits and risks of PSA testing
- The information sheet for well men includes Algorithm 2, which explains the PSA test. It also includes a list of the potential advantages and disadvantages of the PSA test for men to consider when making a decision.

