Overview
A concise summary of recommendations for the diagnosis and management of tree nut and peanut allergies, including recommendations for primary care settings and schools.
Epidemiology
- Peanut and tree nut allergies are characterised by IgE-mediated reactions to nut proteins
- Primary nut allergy affects 2% of children and 0.5% of adults in the UK
- Infants with severe eczema and/or egg allergy have a higher risk of developing peanut allergy
- Primary nut allergy presents most commonly in the first five years of life, often after the first known ingestion, with typical rapid-onset IgE-mediated symptoms.
Diagnosis
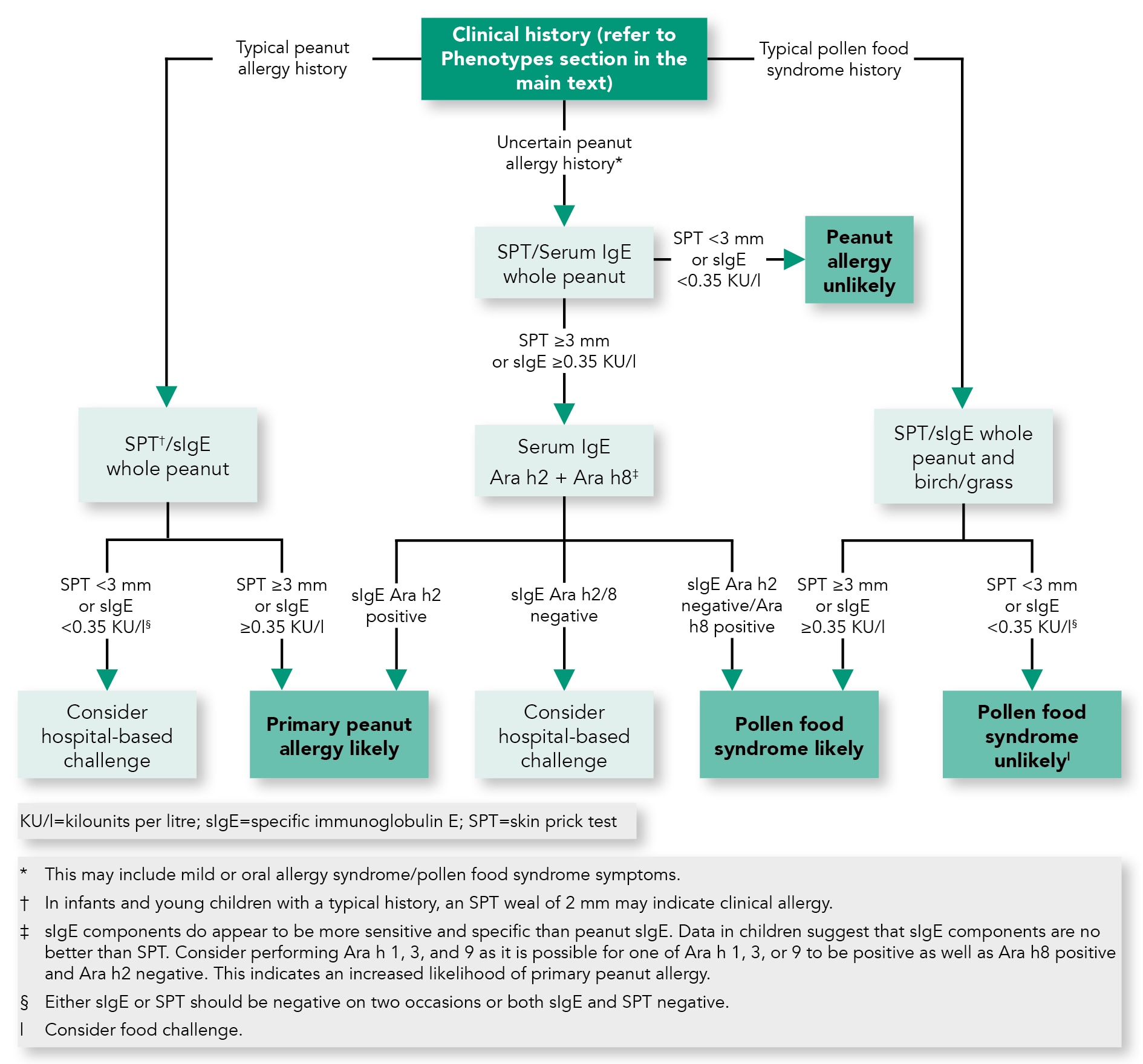
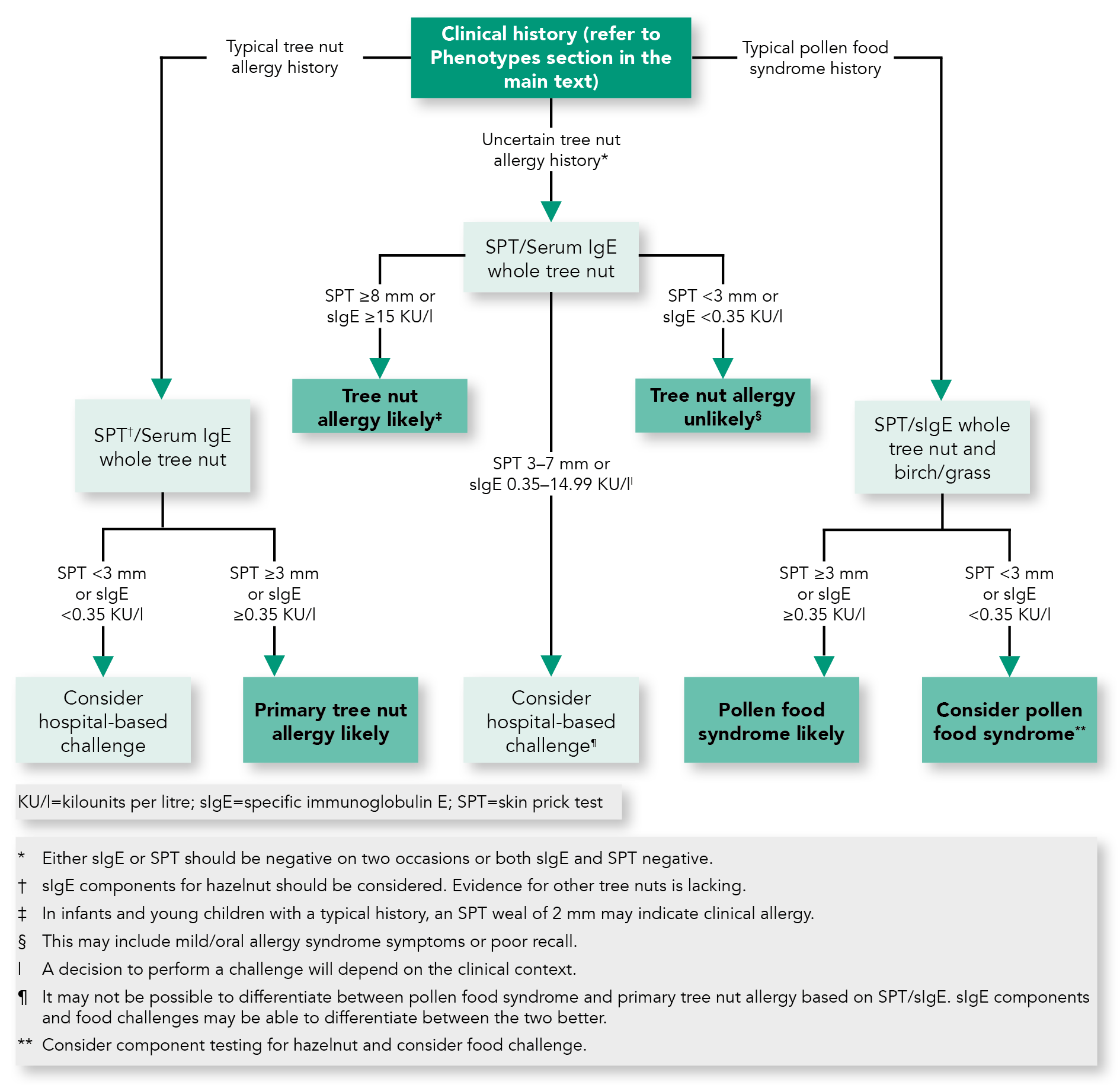
- The clinical diagnosis of primary nut allergy can be made by the combination of a typical clinical presentation and evidence of nut-specific IgE shown by positive skin prick tests (SPTs) or specific IgE (sIgE) test (see figures 1 and 2)
- Pollen food syndrome is a distinct disorder, usually mild, with oral/pharyngeal symptoms, in the context of hayfever or pollen sensitisation, which can be triggered by nuts. It can usually be distinguished clinically from primary nut allergy
- The magnitude of a SPT or sIgE result relates to the probability of clinical allergy but not to clinical severity
- SPT of ≥8 mm or sIgE ≥15 KU/L to peanut is highly predictive of clinical allergy. Cut-off values are not available for tree nuts. Test results should be interpreted in the context of the clinical history
- Diagnostic food challenges are usually not necessary but may be used to confirm or refute the diagnosis when history and test results are conflicting.
Management
- Nut allergy is likely to be a long-lived disease; nut avoidance advice is the cornerstone of management
- Referral to a specialist allergy service is usually required. Patients should be provided with a comprehensive management plan including avoidance advice, patient-specific emergency medication and an emergency treatment plan, and training in administration of emergency medication. Regular retraining is required
- As part of the comprehensive management plans for children, all staff within the school and early years setting require appropriate training in managing an allergic reaction
- Nut allergy can lead to significant psychological burden as well as social and dietary restrictions that may affect quality of life.
Phenotypes
- Primary nut allergy is characterised by systemic and often severe reactions to nuts in patients with specific IgE against the major storage proteins, e.g. Ara h2 for peanut
- Pollen food syndrome, also known as oral allergy syndrome is characterised by seasonal allergic rhinitis and a history of reactions to fresh fruit, vegetables or nuts. Symptoms are typically mild and isolated to the oropharynx. Anaphylaxis can occur but is uncommon. Serum specific IgE is directed against heat-labile proteins (PR-10 homologues) homologous to those in pollen, e.g. Ara h 8 for peanut.
Algorithm 1: Suggested Algorithm for the Diagnosis of Peanut Allergy
Algorithm 2: Suggested Algorithm for the Diagnosis of Tree Nut Allergy
Management at Follow-up Appointments
- Take history of reactions to inadvertent exposure to nut and identification of new allergies
- Provision of ongoing education on nut avoidance measures
- Resolution of nut allergy—periodic measurement of nut SPT +/- nut sIgE. Resolution may have occurred if there has been no reaction following accidental ingestion or there has been a significant reduction in SPT/sIgE (see figures 1 and 2). Testing can also be used to determine tolerance or allergy to other nut
- Training for emergency treatment of accidental reactions, including reviewing written emergency action plans and AAI retraining. Emphasis on carrying AAI on person at all times
- Management of co-morbidities, especially asthma (including asthma management plan), rhinitis and eczema.
Recommendations for Schools
Adapted from Muraro A, Clark A, Beyer K et al. The management of the allergic child at school: EAACI/GA2LEN Task Force on the allergic child at school. Allergy 2010; 65: 681–689.- Ensure there is a system to identify food-allergic children to staff, especially catering or new/temporary staff
- Clear allergen labeling should be available for any food provided by the school. Menus could be made available to the family in advance with ingredients clearly stated
- Staff should be made aware of how to handle potential food allergens safely, including effective cleaning of surfaces and utensils
- Schools should consider the impact of provision of foods containing nuts on nut allergic children
- Discourage trading or sharing food, and sharing utensils or containers
- Ensure lessons avoid the use of provoking food allergens (e.g. using peanuts during science or art lessons)
- Educate staff and pupils regarding allergen avoidance and recognition of food allergy reactions
- Separating children from their peers during mealtimes is unnecessary, provided the other measures described are instituted.

