Latest Guidance UpdatesMarch 2023: added information on Epiduo in the table listing advantages and disadvantages of treatment options. |
Overview
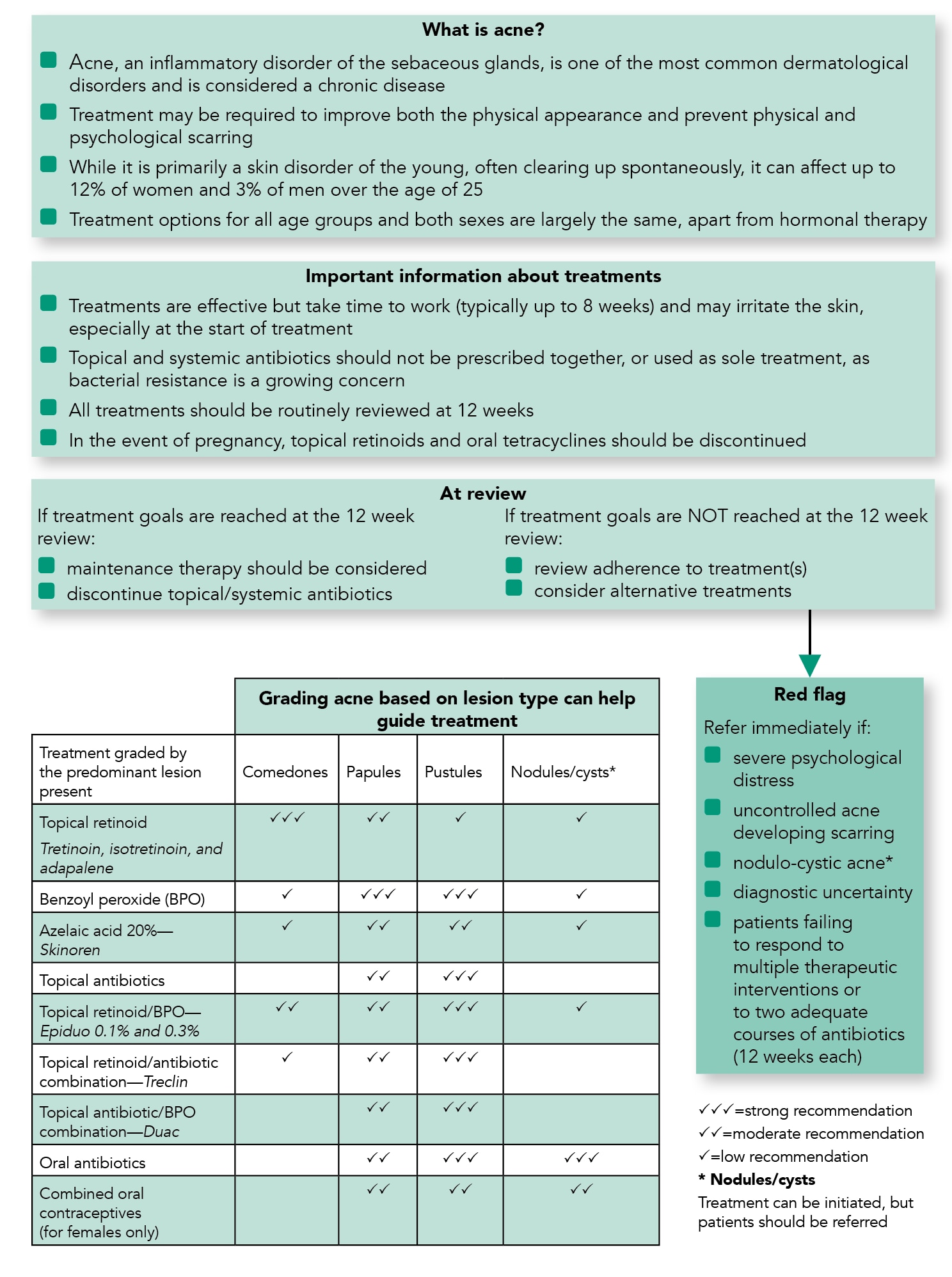
This is a summary of the Primary Care Dermatology Society (PCDS) guidance on the treatment of acne in primary care. It includes a primary care treatment pathway, practical advice, maintenance advice, and top tips and myth busting.
Reflecting on Your Learnings
Reflection is important for continuous learning and development, and a critical part of the revalidation process for UK healthcare professionals. Click here to access the Guidelines Reflection Record.
Primary Care Treatment Pathway
Algorithm 1: PCDS Acne Primary Care Treatment Pathway
Practical Advice
- Topical retinoids should be used for all grades of acne. Adapalene is better tolerated than other topical retinoids. Topical retinoids are contraindicated in pregnancy
- The irritant reaction with topical retinoids and benzoyl peroxide (BPO) can be ameliorated by gradual introduction, for example, by short contact initially (tea time to bed time) or less frequent application (two or three times a week). Concurrent use with light noncomedogenic emollients may be useful
- Azelaic acid may be beneficial in patients with darker skin, in which acne can lead to hyperpigmentation
- BPO can cause bleaching of fabric
- Oral antibiotics should not be used as sole treatment. They should be prescribed with a topical retinoid and/or a BPO. Tetracyclines are first line and all show similar efficacy. Lymecycline and doxycycline are likely to have better adherence because of their once-daily dosage. Minocycline should not normally be used in view of its higher risks. No tetracycline should be used in those aged under 12 years. Erythromycin is second line (first line in pregnancy and in children) owing to its high bacterial resistance. Trimethoprim is an option, but uncommonly used in primary care
- Oral contraceptives: unopposed progesterones (including LARCs) can make acne worse. Second- and third-generation combined oral contraceptives are generally preferred. Co-cyprindiol (Dianette) is used in moderate-to-severe acne when other treatments have failed, and discontinued 3 months after the acne has been controlled
- Combination products: Combining topical treatments is recommended for most people with moderate acne (ref: NICE CKS). Combination products improve adherence
Table 1: Overview of Combination Products for the Treatment of Acne
| Advantages | Disadvantages | |
|---|---|---|
| Epiduo |
|
|
| Treclin |
|
|
| Duac |
|
|
Maintenance
- As acne is a chronic condition, it is advisable to use a topical retinoid for long-term maintenance. This may mean years. Occasional flares may require revisiting previously successful treatments
| Box 1: Top Tips and Myth Busting |
|---|
|
| GI=glycaemic index |

