Overview
This Guidelines summary sets out an antimicrobial prescribing strategy for secondary bacterial infection of eczema and covers infection of other common skin conditions. It aims to optimise antibiotic use and reduce antibiotic resistance. The recommendations are for adults, young people, and children aged 72 hours and over. They do not cover diagnosis.
This guideline updates and replaces some recommendations on managing infections in the NICE guideline on atopic eczema in under 12s.
The recommendations in this guideline were developed before the COVID-19 pandemic.
Managing Secondary Bacterial Infections of Eczema
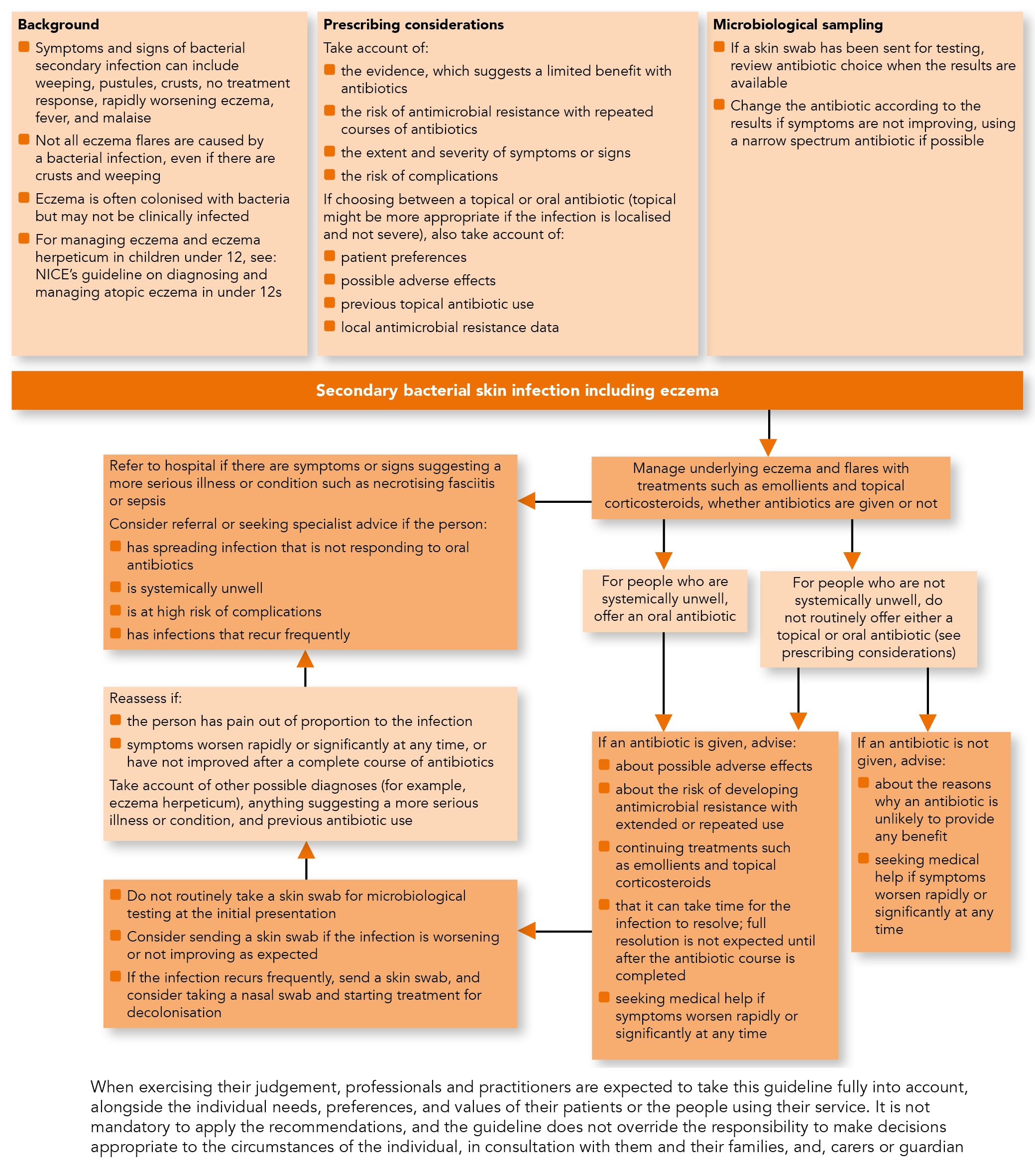
Algorithm 1: Secondary Bacterial Infection of Eczema: Antimicrobial Prescribing
Treatment
- In people with symptoms or signs of cellulitis, follow the NICE guideline on cellulitis and erysipelas: antimicrobial prescribing
- Manage underlying eczema and flares with treatments such as emollients and topical corticosteroids, whether antibiotics are offered or not (see the NICE guideline on atopic eczema in under 12s and also see NICE’s technology appraisal guidance on alitretinoin for the treatment of severe chronic hand eczema, dupilumab for treating moderate to severe atopic dermatitis, tacrolimus and pimecrolimus for atopic eczema, and frequency of application of topical corticosteroids for atopic eczema)
- Be aware that:
- the symptoms and signs of secondary bacterial infection of eczema can include:
- weeping
- pustules
- crusts
- no response to treatment
- rapidly worsening eczema
- fever and malaise
- not all eczema flares are caused by a bacterial infection, so will not respond to antibiotics, even if weeping and crusts are present
- eczema is often colonised with bacteria but may not be clinically infected
- eczema can also be infected with herpes simplex virus (eczema herpeticum). For managing eczema and eczema herpeticum in children under 12, see the NICE guideline on atopic eczema in under 12s
- the symptoms and signs of secondary bacterial infection of eczema can include:
- Do not routinely take a skin swab for microbiological testing in people with secondary bacterial infection of eczema at the initial presentation
- In people who are not systemically unwell, do not routinely offer either a topical or oral antibiotic for secondary bacterial infection of eczema. Take into account:
- the evidence, which suggests a limited benefit with antibiotics in addition to topical corticosteroids compared with topical corticosteroids alone
- the risk of antimicrobial resistance with repeated courses of antibiotics
- the extent and severity of symptoms or signs
- the risk of developing complications, which is higher in people with underlying conditions such as immunosuppression
- If an antibiotic is offered to people who are not systemically unwell with a secondary bacterial infection of eczema when choosing between a topical or oral antibiotic, take into account:
- their preferences (and those of their parents and carers as appropriate) for topical or oral administration
- the extent and severity of symptoms or signs (a topical antibiotic may be more appropriate if the infection is localised and not severe; an oral antibiotic may be more appropriate if the infection is widespread or severe)
- possible adverse effects
- previous use of topical antibiotics because antimicrobial resistance can develop rapidly with extended or repeated use
- In people who are systemically unwell, offer an oral antibiotic for secondary bacterial infection of eczema.
Advice
- If an antibiotic is not given, advise the person (and their parents and carers as appropriate):
- about the reasons why an antibiotic is unlikely to provide any benefit
- to seek medical help if symptoms worsen rapidly or significantly at any time
- If an antibiotic is given, advise the person (and their parents and carers as appropriate):
- about possible adverse effects
- about the risk of developing antimicrobial resistance with extended or repeated use
- that they should continue treatments such as emollients and topical corticosteroids
- that it can take time for secondary bacterial infection of eczema to resolve, and full resolution is not expected until after the antibiotic course is completed
- to seek medical help if symptoms worsen rapidly or significantly at any time.
Reassessment
- Reassess people with secondary bacterial infection of eczema if:
- they become systemically unwell, or have pain that is out of proportion to the infection
- their symptoms worsen rapidly or significantly at any time
- their symptoms have not improved after completing a course of antibiotics
- When reassessing people with secondary bacterial infection of eczema, take account of:
- other possible diagnoses, such as eczema herpeticum
- any symptoms or signs suggesting a more serious illness or condition, such as cellulitis, necrotising fasciitis, or sepsis
- previous antibiotic use, which may have caused resistant bacteria
- For people with secondary bacterial infection of eczema that is worsening or has not improved as expected, consider sending a skin swab for microbiological testing
- For people with secondary bacterial infection of eczema that recurs frequently:
- send a skin swab for microbiological testing and
- consider taking a nasal swab and starting treatment for decolonisation
- If a skin swab has been sent for microbiological testing:
- review the choice of antibiotic when results are available and
- change the antibiotic according to results if symptoms are not improving, using a narrow-spectrum antibiotic if possible.
Referral and seeking specialist advice
- Refer people with secondary bacterial infection of eczema to hospital if they have any symptoms or signs suggesting a more serious illness or condition, such as necrotising fasciitis or sepsis
- Consider referral or seeking specialist advice for people with secondary bacterial infection of eczema if they:
- have spreading infection that is not responding to oral antibiotics
- are systemically unwell
- are at high risk of complications
- have infections that recur frequently.
Choice of Antibiotic
- When prescribing an antibiotic for secondary bacterial infection of eczema, take account of local antimicrobial resistance data when available and follow:
- Table 1 for adults aged 18 years and over
- Table 2 for children and young people under 18 years (for children under 1 month, antibiotic choice is based on specialist advice).
Table 1: Choice of Antibiotics for Adults Aged 18 Years and Over
| Treatment | Antibiotic, Dosage, and Course Length |
|---|---|
| For secondary bacterial infection of eczema in people who are not systemically unwell | Do not routinely offer either a topical or oral antibiotic |
| First-choice topical if a topical antibiotic is appropriate | Fusidic acid 2%:
|
| First-choice oral if an oral antibiotic is appropriate | Flucloxacillin:
|
| Alternative oral antibiotic if the person has a penicillin allergy or flucloxacillin is unsuitable | Clarithromycin:
|
| Alternative oral antibiotic if the person has a penicillin allergy or flucloxacillin is unsuitable, and the person is pregnant | Erythromycin:
|
| If methicillin-resistant Staphylococcus aureus is suspected or confirmed | Consult a microbiologist |
| See the British National Formulary for appropriate use and dosing of the antibiotics recommended in specific populations, for example, people with hepatic or renal impairment, and in pregnancy and breastfeeding | |
Table 2: Choice of Antibiotics for Children and Young People Aged From 1 Month to Under 18 years
| Treatment | Antibiotic, Dosage, and Course Length |
|---|---|
| For secondary bacterial infection of eczema in people who are not systemically unwell | Do not routinely offer either a topical or oral antibiotic |
| First-choice topical if a topical antibiotic is appropriate | Fusidic acid 2%:
|
| First-choice oral if an oral antibiotic is appropriate | Flucloxacillin (oral solution or capsules):
|
| Alternative oral antibiotic if the person has a penicillin allergy or flucloxacillin is unsuitable | Clarithromycin:
|
| Alternative oral antibiotic if the person has a penicillin allergy or flucloxacillin is unsuitable, and the person is pregnant | Erythromycin:
|
| If methicillin-resistant Staphylococcus aureus is suspected or confirmed | Consult a local microbiologist |
| See the British National Formulary for Children for appropriate use and dosing of the antibiotics recommended in specific populations, for example, people with hepatic or renal impairment, and in pregnancy and breastfeedingThe age bands for children apply to children of average size. In practice, they will be used alongside other factors such as the severity of the condition being treated and the child’s size in relation to the average size of children of the same age For advice on helping children to swallow medicines, see Medicines for Children’s leaflet on helping your child to swallow tablets | |
Managing Secondary Bacterial Infections of Psoriasis, Chickenpox, Shingles, and Scabies
Treatment
- Be aware that no evidence was found on the use of antibiotics in managing secondary bacterial infections of other common skin conditions such as psoriasis, chickenpox, shingles, and scabies. Seek specialist advice, if needed.

