This Guidelines summary sets out an antimicrobial prescribing strategy for adults with leg ulcer infection. It aims to optimise antibiotic use and reduce antibiotic resistance.
This summary only covers key recommendations for primary care. For a complete set of recommendations, see the full guideline.
Algorithm 1: Leg Ulcer Infection: Antimicrobial Prescribing
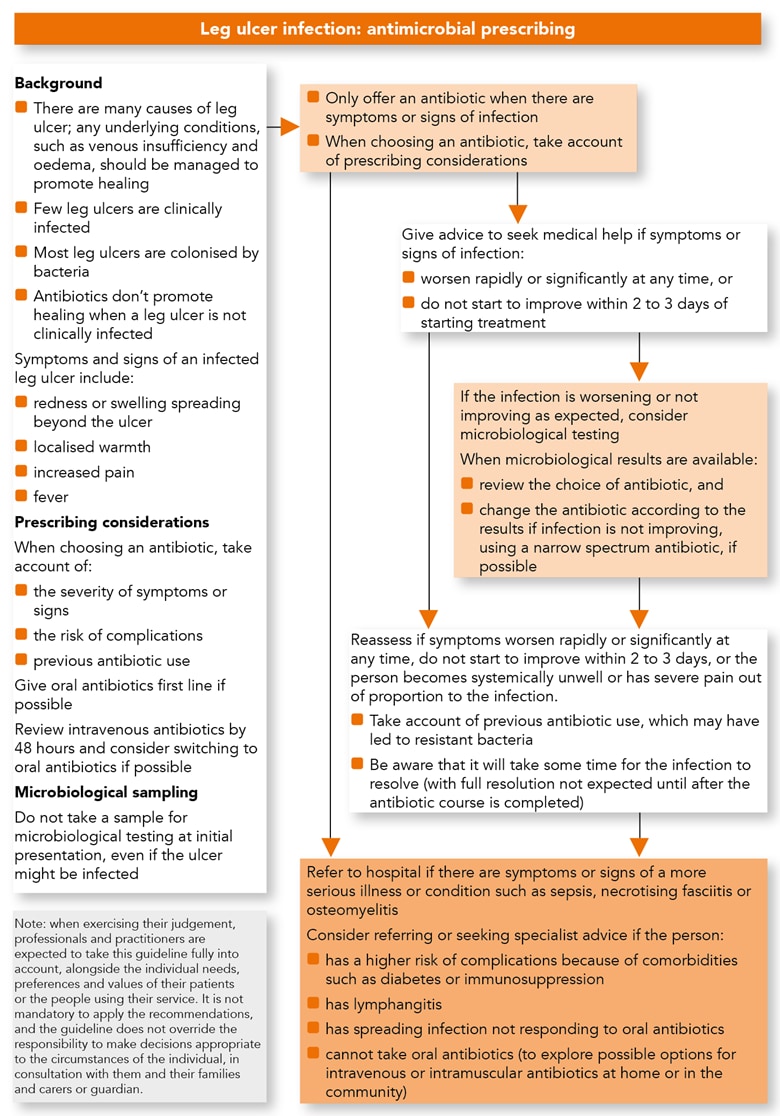
Managing Leg Ulcer Infection in Adults
Treatment
- Be aware that:
- there are many causes of leg ulcers: underlying conditions, such as venous insufficiency and oedema, should be managed to promote healing
- most leg ulcers are not clinically infected but are likely to be colonised with bacteria
- antibiotics do not help to promote healing when a leg ulcer is not clinically infected
- Do not take a sample for microbiological testing from a leg ulcer at initial presentation, even if it might be infected
- Only offer an antibiotic for adults with a leg ulcer when there are symptoms or signs of infection (for example, redness or swelling spreading beyond the ulcer, localised warmth, increased pain or fever). When choosing an antibiotic (see the recommendations on choice of antibiotic) take account of:
- the severity of symptoms or signs
- the risk of developing complications
- previous antibiotic use
- Give oral antibiotics if the person can take oral medicines, and the severity of their condition does not require intravenous antibiotics
- If intravenous antibiotics are given, review by 48 hours and consider switching to oral antibiotics if possible
Advice
- When prescribing antibiotics for an infected leg ulcer in adults, give advice to seek medical help if symptoms or signs of the infection worsen rapidly or significantly at any time, or do not start to improve within 2 to 3 days of starting treatment
Reassessment
- Reassess an infected leg ulcer in adults if:
- symptoms or signs of the infection worsen rapidly or significantly at any time, or do not start to improve within 2 to 3 days
- the person becomes systemically unwell or has severe pain out of proportion to the infection
- When reassessing an infected leg ulcer in adults, take account of previous antibiotic use, which may have led to resistant bacteria
- Be aware that it will take some time for a leg ulcer infection to resolve, with full resolution not expected until after the antibiotic course is completed
- Consider sending a sample from the leg ulcer (after cleaning) for microbiological testing if symptoms or signs of the infection are worsening or have not improved as expected
- When microbiological results are available:
- review the choice of antibiotic(s) and
- change the antibiotic(s) according to results if symptoms or signs of the infection are not improving, using a narrow-spectrum antibiotic if possible
Referral or Seeking Specialist Advice
- Refer adults with an infected leg ulcer to hospital if they have any symptoms or signs suggesting a more serious illness or condition, such as sepsis, necrotising fasciitis or osteomyelitis
- Consider referring or seeking specialist advice for adults with an infected leg ulcer if they:
- have a higher risk of complications because of comorbidities, such as diabetes or immunosuppression
- have lymphangitis
- have spreading infection that is not responding to oral antibiotics
- cannot take oral antibiotics (exploring locally available options for giving intravenous or intramuscular antibiotics at home or in the community, rather than in hospital, where appropriate)
Choice of Antibiotic
- When prescribing antibiotics for an infected leg ulcer in adults aged 18 years and over, follow the recommendations in Table 1 below.
Table 1: Antibiotics for Adults Aged 18 Years and Over
| Antibiotic[A] | Dosage and course length[B] |
|---|---|
| First‑choice oral antibiotic | |
| Flucloxacillin | 500 mg to 1 g[C],[D] 4 times a day for 7 days |
| Alternative first‑choice oral antibiotics for penicillin allergy or if flucloxacillin unsuitable | |
| Doxycycline | 200 mg on first day, then 100 mg once a day (can be increased to 200 mg daily) for 7 days in total |
| Clarithromycin | 500 mg twice a day for 7 days |
| Erythromycin (in pregnancy) | 500 mg 4 times a day for 7 days |
| Second‑choice oral antibiotics (guided by microbiological results when available) | |
| Co-amoxiclav | 500/125 mg 3 times a day for 7 days |
| Co-trimoxazole[D],[E],[F] (in penicillin allergy) | 960 mg twice a day for 7 days |
| First‑choice antibiotics if severely unwell (guided by microbiological results if available)[G] | |
| Flucloxacillin with or without | 1–2 g 4 times a day IV |
| Gentamicin[F],[H]and/or | Initially 5–7 mg/kg IV, subsequent doses if required adjusted according to serum gentamicin concentration |
| Metronidazole | 400 mg 3 times a day orally or 500 mg 3 times a day IV |
| Co-amoxiclav with or without | 1.2 g 3 times a day IV |
| Gentamicin[F],[H] | Initially 5–7 mg/kg IV, subsequent doses if required adjusted according to serum gentamicin concentration |
| Co-trimoxazole[D],[E],[F] (in penicillin allergy) with or without | 960 mg twice a day IV (increased to 1.44 g twice a day if severe infection) |
| Gentamicin[F],[H]and/or | Initially 5–7 mg/kg IV, subsequent doses if required adjusted according to serum gentamicin concentration |
| Metronidazole | 400 mg 3 times a day orally or 500 mg 3 times a day IV |
| Second‑choice antibiotics if severely unwell (guided by microbiological results when available or following specialist advice)[G] | |
| Piperacillin with tazobactam | 4.5 g 3 times a day IV (increased to 4.5 g 4 times a day if severe infection) |
| Ceftriaxone with or without | 2 g once a day IV |
| Metronidazole | 400 mg 3 times a day orally or 500 mg 3 times a day IV |
| Antibiotics to be added if MRSA infection is suspected or confirmed (combination therapy with antibiotics listed above)[G]Antibiotics to be added if MRSA infection is suspected or confirmed (combination therapy with antibiotics listed above)[G] | |
| Vancomycin[F],[H] | 15–20 mg/kg 2 or 3 times a day IV (maximum 2 g per dose), adjusted according to serum vancomycin concentration |
| Teicoplanin[F],[H] | Initially 6 mg/kg every 12 hours for 3 doses, then 6 mg/kg once a day IV |
| Linezolid (if vancomycin or teicoplanin cannot be used; specialist advice only)[F] | 600 mg twice a day orally or IV |
| [A] See BNF for appropriate use and dosing in specific populations, for example, hepatic impairment, renal impairment, pregnancy and breastfeeding, and administering IV (or, when appropriate, intramuscular) antibiotics. [B] Oral doses are for immediate‑release medicines. [C] The upper dose of 1 g 4 times a day would be off-label, as defined in the NICE glossary. [D] The prescriber should follow relevant professional guidance, taking full responsibility for the decision. Informed consent should be obtained and documented. See the General Medical Council’s good practice in prescribing and managing medicines and devices for further information. [E] Not licensed for leg ulcer infection, so use would be off-label. [F] See BNF for information on monitoring of patient parameters. [G] Review IV antibiotics by 48 hours and consider switching to oral antibiotics if possible. [H] See BNF for information on therapeutic drug monitoring. | |
| Abbreviations: IV=intravenous; MRSA=methicillin-resistant Staphylococcus aureus. | |

