This summary provides an antimicrobial prescribing strategy for human and animal bites (excluding insect bites) in adults, young people, and children aged 72 hours and over. It aims to optimise antibiotic use and reduce antibiotic resistance.
It includes a visual summary of the recommendations, including tables to support prescribing decisions.
The recommendations in this guideline were developed before the COVID-19 pandemic. The guideline is aimed at healthcare professionals, people with a human or animal bite, their families and carers and it may also be relevant for veterinary professionals.
Click here for a summary of antimicrobial prescribing guidance for insect bites and stings.
Read the related Guidelines in Practice article Bites and Stings: When to Prescribe an Antibiotic.
Managing Human and Animal Bites
Assessment
- For people with a human or animal bite:
- assess the type and severity of the bite, including what animal caused the bite, the site and depth of the wound, and whether it is infected (see the recommendation on taking a swab in the section on treating infected bites)
- assess the risk of tetanus, rabies or a bloodborne viral infection and take appropriate action
- manage the wound with irrigation and debridement as necessary
- be aware of potential safeguarding issues in vulnerable adults and children, for example, as outlined in NICE’s guidelines on child maltreatment,challenging behaviour and learning disabilities and domestic violence and abuse.
- Seek specialist advice from a microbiologist for bites from a wild or exotic animal (including birds and non-traditional pets) because the spectrum of bacteria involved may be different, and there may be a risk of other serious nonbacterial infections
- Consider seeking specialist advice from a microbiologist for domestic animal bites (including farm animal bites), that you are unfamiliar with.
Antibiotic Prophylaxis for Uninfected Bites
Human Bites
- Do not offer antibiotic prophylaxis to people with a human bite that has not broken the skin
- Offer antibiotic prophylaxis (see the recommendation on choice of antibiotic) to people with a human bite that has broken the skin and drawn blood
- Consider antibiotic prophylaxis for people with a human bite that has broken the skin but not drawn blood if it:
- involves a high-risk area such as the hands, feet, face, genitals, skin overlying cartilaginous structures or an area of poor circulation or
- is in a person at risk of a serious wound infection because of a comorbidity (such as diabetes, immunosuppression, asplenia or decompensated liver disease).
Cat Bites
- Do not offer antibiotic prophylaxis to people with a cat bite that has not broken the skin
- Offer antibiotic prophylaxis to people with a cat bite that has broken the skin and drawn blood
- Consider antibiotic prophylaxis for people with a cat bite that has broken the skin but not drawn blood if the wound could be deep.
Bites from a Dog or Other Traditional Pet (Excluding Cat Bites)
- Do not offer antibiotic prophylaxis to people with a bite from a dog or other traditional pet (excluding cat bites) that:
- has not broken the skin or
- has broken the skin but not drawn blood.
- Offer antibiotic prophylaxis to people with a bite from a dog or other traditional pet (excluding cat bites) that has broken the skin and drawn blood if it
- has penetrated bone, joint, tendon or vascular structures or
- is deep, is a puncture or crush wound, or has caused significant tissue damage or
- is visibly contaminated (for example, if there is dirt or a tooth in the wound).
- Consider antibiotic prophylaxis for people with a bite from a dog or other traditional pet (excluding cat bites) that has broken the skin and drawn blood if it:
- involves a high-risk area such as the hands, feet, face, genitals, skin overlying cartilaginous structures or an area of poor circulation or
- is in a person at risk of a serious wound infection because of a comorbidity (such as diabetes, immunosuppression, asplenia or decompensated liver disease).
Treating Infected Bites
- Take a swab for microbiological testing to guide treatment if there is discharge (purulent or non-purulent) from the human or animal bite wound
- Offer an antibiotic (see the recommendations on choice of antibiotic) for people with a human or animal bite if there are symptoms or signs of infection, such as increased pain, inflammation, fever, discharge or an unpleasant smell.
Advice
- Give advice to people with a human or animal bite about:
- possible adverse effects of antibiotics (if they have been offered antibiotics)
- seeking medical help if symptoms or signs of infection develop or worsen rapidly or significantly at any time, or do not start to improve within 24 to 48 hours of starting treatment.
Reassessment
- Reassess the human or animal bite if:
- symptoms or signs of infection develop or worsen rapidly or significantly at any time, or do not start to improve within 24 to 48 hours of starting treatment or
- the person becomes systemically unwell or
- the person has severe pain that is out of proportion to the infection
- Be aware that people who have difficulty communicating may have non-verbal signs of pain, such as a change in behaviour
- If a skin swab has been sent for microbiological testing, review the choice of antibiotic based on the swab results. If a change of antibiotic is needed, use a narrow-spectrum antibiotic if possible.
Referral and Seeking Specialist Advice
- Refer people with a human or animal bite to hospital if they have:
- symptoms or signs suggesting a more serious illness or condition (these include severe cellulitis, abscess, osteomyelitis, septic arthritis, necrotising fasciitis or sepsis) or
- a penetrating wound involving arteries, joints, nerves, muscles, tendons, bones or the central nervous system
- Consider referral or seeking specialist advice for people with a human or animal bite if:
- they are systemically unwell or
- they have developed symptoms or signs of infection after taking prophylactic antibiotics or
- they have lymphangitis or
- they are at risk of a serious wound infection because of a pre-existing medical condition or
- they cannot take oral antibiotics (in which case, explore with the specialist whether locally available options for parenteral antibiotics at home or in the community, rather than in hospital, are appropriate) or
- the bite is infected and is not responding to oral antibiotics or
- the bite is in an area of poor circulation.
Choice of Antibiotic
- When prescribing an antibiotic for a bite from a human, cat, dog or other traditional pet:
- follow Table 1 for adults aged 18 years and over
- follow Table 2 for children and young people under 18 years
- Give oral antibiotics if the person can take oral medicines, and the severity of their condition does not need intravenous antibiotics
- If intravenous antibiotics are given, review within 48 hours and consider switching to oral antibiotics if possible.
Algorithm 1: Human and Animal Bites—Antimicrobial Prescribing
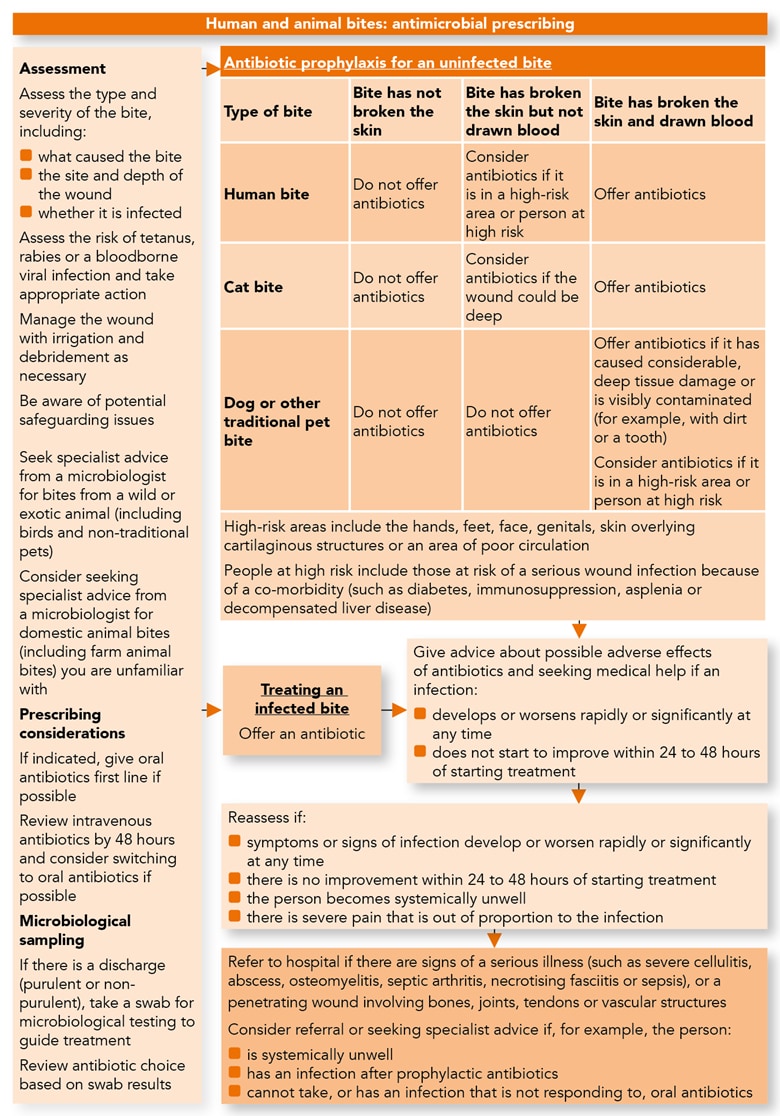
Table 1: Antibiotics for Prophylaxis and Treatment in Adults Aged 18 Years and Over
| Prophylaxis and treatment | Antibiotic, dosage and course length for prophylaxis (3 days) and treatment (5 days) |
|---|---|
| First-choice oral antibiotic | Co-amoxiclav: 250/125 mg or 500/125 mg three times a day |
| Alternative first-choice oral antibiotics for penicillin allergy or if co-amoxiclav is unsuitable | Doxycycline: 200 mg on first day, then 100 mg or 200 mg daily with Metronidazole: 400 mg three times a day |
| Alternative first-choice oral antibiotics in pregnancy for penicillin allergy or if co-amoxiclav is unsuitable | Seek specialist advice |
| First-choice intravenous antibiotic (if unable to take oral antibiotics or severely unwell) | Co-amoxiclav: 1.2 g three times a day |
| Alternative first-choice intravenous antibiotics for penicillin allergy or if co-amoxiclav is unsuitable | Cefuroxime (caution in penicillin allergy): 750 mg three times a day (increased to 750 mg four times a day or 1.5 g three or four times a day if infection is severe) with Metronidazole: 500 mg three times a day Ceftriaxone (caution in penicillin allergy): 2 g once a day with Metronidazole: 500 mg three times a day |
| If cephalosporin is not appropriate | Seek specialist advice |
| See the BNF and summary of product characteristics for appropriate use and dosing in specific populations, for example, for people with hepatic or renal impairment, in pregnancy and breastfeeding, and when administering intravenous (or, if appropriate, intramuscular) antibiotics. A 5-day course is appropriate for treating most human or animal bites, but course length can be increased to 7 days (with review) based on clinical assessment of the wound, for example, if there is significant tissue destruction or it has penetrated bone, joint, tendon or vascular structures. | |
Table 2: Antibiotics for Prophylaxis and Treatment in Children and Young People Under 18 Years
| Prophylaxis and treatment | Antibiotic, dosage and course length for prophylaxis (3 days) and treatment (5 days) |
|---|---|
| Choice for children under 1 month | Seek specialist advice |
| First-choice oral antibiotic for children aged 1 month and over | Co-amoxiclav: 1 month to 11 months: 0.25 ml/kg of 125/31 suspension three times a day 1 year to 5 years: 0.25 ml/kg or 5 ml of 125/31 suspension three times a day 6 years to 11 years: 0.15 ml/kg or 5 ml of 250/62 suspension three times a day 12 years to 17 years: 250/125 mg or 500/125 mg three times a day Co-amoxiclav 400/57 suspension may also be considered to allow for twice-daily dosing |
| Alternative first-choice oral antibiotic for children under 12 years for penicillin allergy or if co-amoxiclav is unsuitable | Co-trimoxazole (off-label use): 6 weeks to 5 months: 120 mg or 24 mg/kg twice a day 6 months to 5 years: 240 mg or 24 mg/kg twice a day 6 years to 11 years: 480 mg or 24 mg/kg twice a day See the BNF for Children for information on monitoring |
| Alternative first-choice oral antibiotics for young people aged 12 to 17 years for penicillin allergy or if co-amoxiclav is unsuitable | Doxycycline: 200 mg on first day, then 100 mg or 200 mg daily with Metronidazole: 400 mg three times a day |
| Alternative first-choice oral antibiotics in pregnancy for penicillin allergy or if co-amoxiclav unsuitable | Seek specialist advice |
| First-choice intravenous antibiotic (if unable to take oral antibiotics or severely ill) | Co-amoxiclav: 1 month to 2 months: 30 mg/kg twice a day 3 months to 17 years: 30 mg/kg three times a day (maximum per dose 1.2 g) |
| Alternative first-choice intravenous antibiotics for penicillin allergy or if co-amoxiclav is unsuitable | Cefuroxime (caution in penicillin allergy): 1 month to 17 years: 20 mg/kg three times a day (maximum 750 mg per dose), which can be increased to 50 mg/kg to 60 mg/kg three or four times a day (maximum per dose 1.5 g) with Metronidazole: 1 month: loading dose 15 mg/kg, then (after 8 hours) 7.5 mg/kg three times a day 2 months to 17 years: 7.5 mg/kg three times a day (maximum per dose 500 mg) Ceftriaxone (caution in penicillin allergy): 1 month to 11 years (up to 50 kg): 50 mg/kg to 80 mg/ kg once a day (maximum 4 g per day) 9 years to 11 years (50 kg and above) and 12 years to 17 years: 1 g to 2 g once a day with Metronidazole: 1 month: loading dose 15 mg/kg, then (after 8 hours) 7.5 mg/kg three times a day 2 months to 17 years: 7.5 mg/kg three times a day (maximum per dose 500 mg) |
| If a cephalosporin is not appropriate | Seek specialist advice |
| See the BNF for Children and summary of product characteristics for appropriate use and dosing in specific populations, for example, for people with hepatic or renal impairment, in pregnancy and breastfeeding, and when administering intravenous (or, if appropriate, intramuscular) antibiotics. A 5-day course is appropriate for treating most human or animal bites, but course length can be increased to 7 days (with review) based on clinical assessment of the wound, for example, if there is significant tissue destruction or it has penetrated bone, joint, tendon or vascular structures. For off-label use, the prescriber should follow relevant professional guidance, taking full responsibility for the decision. Informed consent should be obtained and documented. See the General Medical Council’s good practice in prescribing and managing medicines and devices for further information. | |

