This Guidelines summary covers diagnosing, monitoring, and managing asthma in adults, young people, and children. It aims to improve the accuracy of diagnosis, help people to control their asthma, and reduce the risk of asthma attacks. It does not cover managing severe asthma or acute asthma attacks.
A summary of NICE recommendations managing for chronic asthma can be found here.
Initial Clinical Assessment
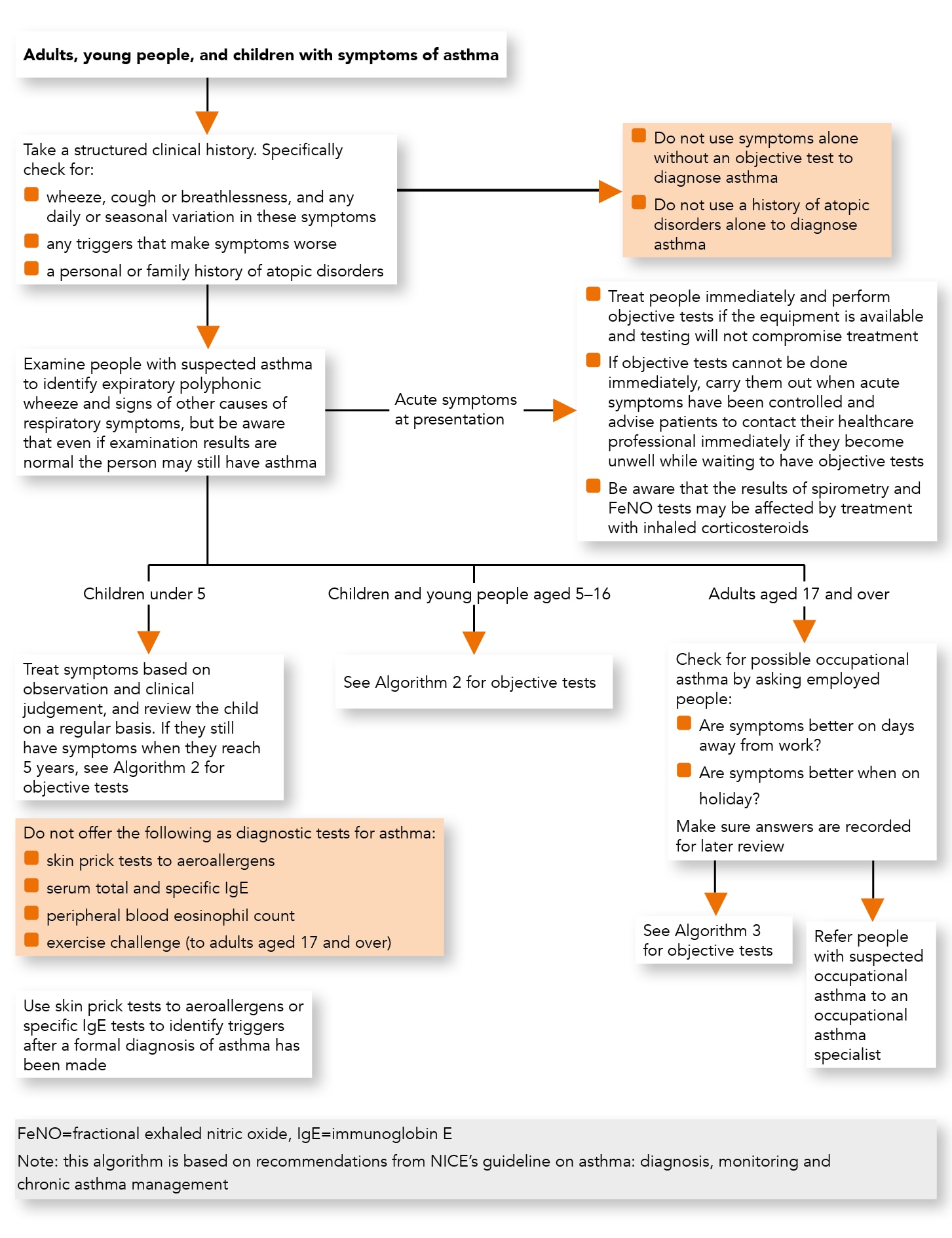
Algorithm 1: Initial Clinical Assessment for Adults, Young People, and Children with Suspected Asthma
Clinical History
- Take a structured clinical history in people with suspected asthma. Specifically, check for:
- wheeze, cough or breathlessness, and any daily or seasonal variation in these symptoms
- any triggers that make symptoms worse
- a personal or family history of atopic disorders
- Do not use symptoms alone without an objective test to diagnose asthma
- Do not use a history of atopic disorders alone to diagnose asthma.
Physical Examination
- Examine people with suspected asthma to identify expiratory polyphonic wheeze and signs of other causes of respiratory symptoms, but be aware that even if examination results are normal the person may still have asthma.
Initial Treatment and Objective Tests for Acute Symptoms at Presentation
- Treat people immediately if they are acutely unwell at presentation, and perform objective tests for asthma (for example, fractional exhaled nitric oxide [FeNO], spirometry, and peak flow variability) if the equipment is available and testing will not compromise treatment of the acute episode
- If objective tests for asthma cannot be done immediately for people who are acutely unwell at presentation, carry them out when acute symptoms have been controlled, and advise people to contact their healthcare professional immediately if they become unwell while waiting to have objective tests
- Be aware that the results of spirometry and FeNO tests may be affected in people who have been treated empirically with inhaled corticosteroids.
Testing for Asthma
- Do not offer the following as diagnostic tests for asthma:
- skin prick tests to aeroallergens
- serum total and specific IgE
- peripheral blood eosinophil count
- exercise challenge (to adults aged 17 and over)
- Use skin prick tests to aeroallergens or specific IgE tests to identify triggers after a formal diagnosis of asthma has been made.
Occupational Asthma
- Check for possible occupational asthma by asking employed people with suspected new-onset asthma, or established asthma that is poorly controlled:
- are symptoms better on days away from work?
- are symptoms better when on holiday (time away from work longer than usual breaks at weekends or between shifts)?
- Make sure all answers are recorded for later review
- Refer people with suspected occupational asthma to an occupational asthma specialist.
Diagnosing Asthma in Young Children
- For children under 5 with suspected asthma, treat symptoms based on observation and clinical judgement, and review the child on a regular basis. If they still have symptoms when they reach 5, carry out objective tests
- If a child is unable to perform objective tests when they are aged 5:
- continue to treat based on observation and clinical judgement
- try doing the tests again every 6–12 months until satisfactory results are obtained
- consider referral for specialist assessment if the child repeatedly cannot perform objective tests and is not responding to treatment.
Objective Tests for Diagnosing Asthma
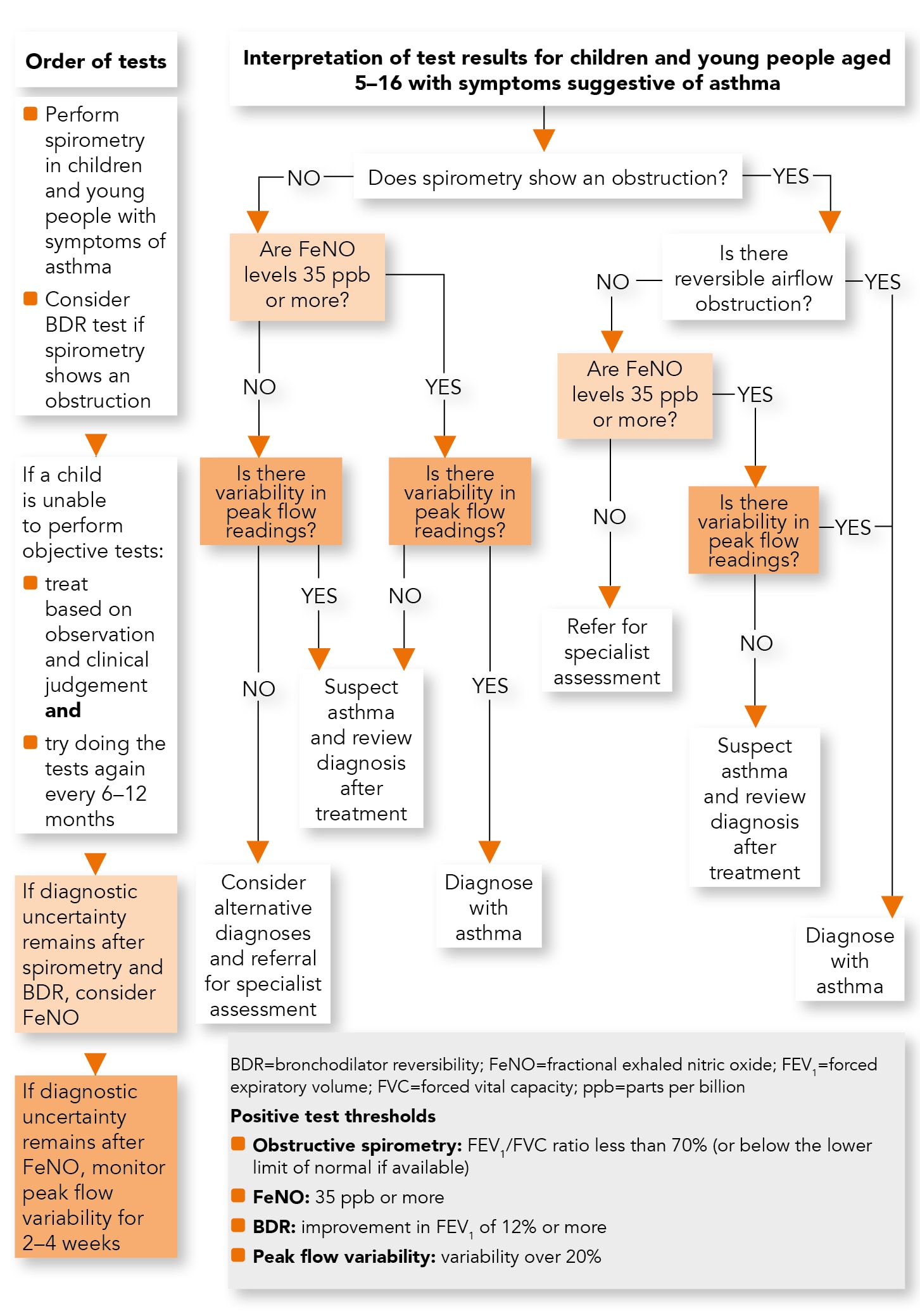
Algorithm 2: Objective Tests for Asthma in Children and Young People aged 5–16
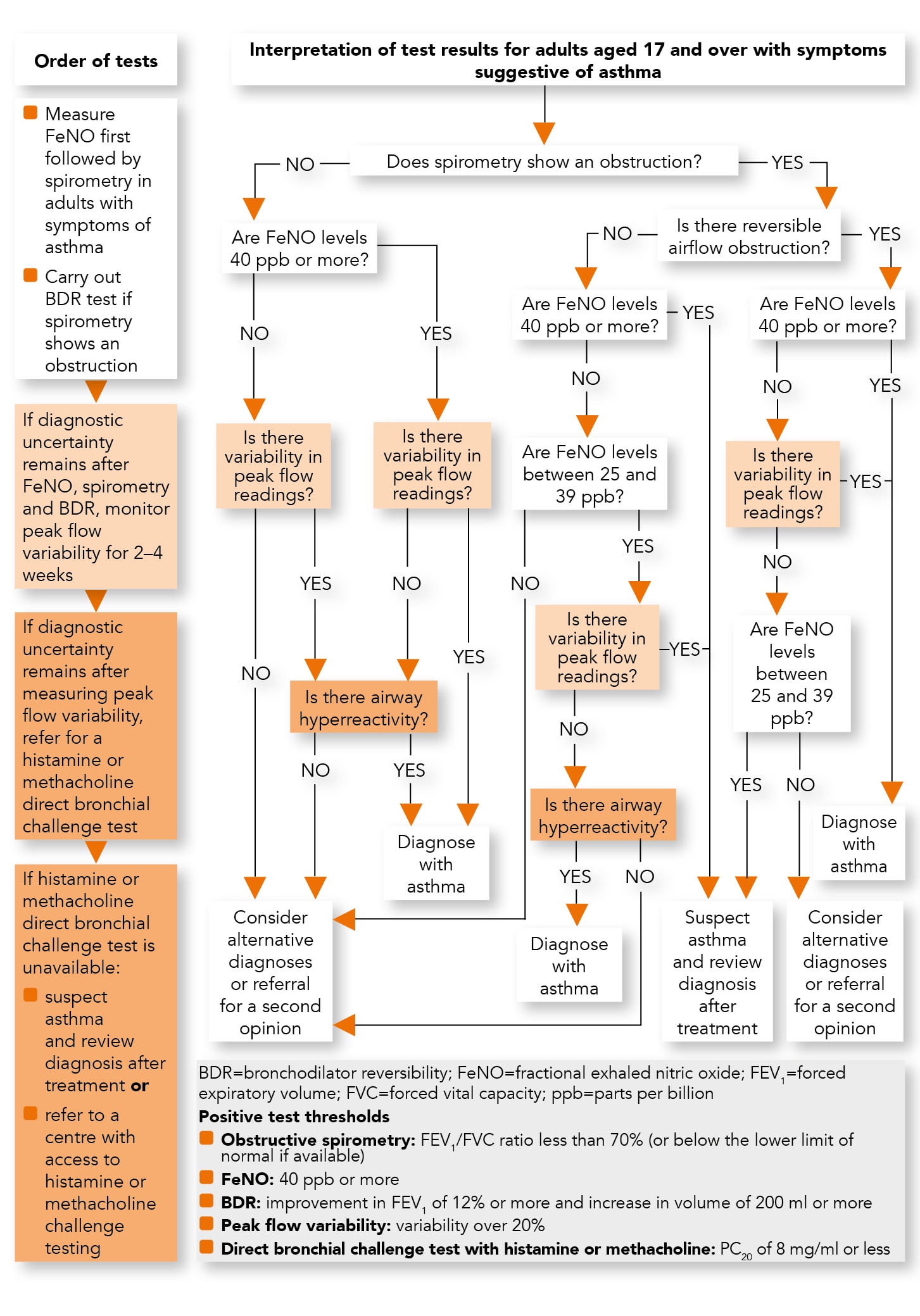
Algorithm 3: Objective Tests for Asthma in Adults aged 17 and Over
Diagnostic Hubs
- Those responsible for planning diagnostic service support to primary care (for example, clinical commissioning groups) should consider establishing asthma diagnostic hubs to achieve economies of scale and improve the practicality of implementing the recommendations in this guideline.
Airway Inflammation Measures
Fractional Exhaled Nitric Oxide
- Offer a FeNO test to adults (aged 17 and over) if a diagnosis of asthma is being considered. Regard a FeNO level of 40 parts per billion (ppb) or more as a positive test
- Consider a FeNO test in children and young people (aged 5–16)[A] if there is diagnostic uncertainty after initial assessment and they have either:
- normal spirometry or
- obstructive spirometry with a negative bronchodilator reversibility (BDR) test.
- Be aware that a person’s current smoking status can lower FeNO levels both acutely and cumulatively. However, a high level remains useful in supporting a diagnosis of asthma.
Lung Function Tests
Spirometry
- Offer spirometry to adults, young people and children aged 5 and over if a diagnosis of asthma is being considered. Regard a forced expiratory volume in 1 second/forced vital capacity (FEV1/FVC) ratio of less than 70% (or below the lower limit of normal if this value is available) as a positive test for obstructive airway disease (obstructive spirometry).
Bronchodilator Reversibility
- Offer a BDR test to adults (aged 17 and over) with obstructive spirometry (FEV1/FVC ratio less than 70%). Regard an improvement in FEV1 of 12% or more, together with an increase in volume of 200 ml or more, as a positive test
- Consider a BDR test in children and young people (aged 5–16) with obstructive spirometry (FEV1/FVC ratio less than 70%). Regard an improvement in FEV1 of 12% or more as a positive test.
Peak Expiratory Flow Variability
- Monitor peak flow variability for 2–4 weeks in adults (aged 17 and over) if there is diagnostic uncertainty after initial assessment and a FeNO test and they have either:
- normal spirometry or
- obstructive spirometry, reversible airways obstruction (positive BDR) but a FeNO level of 39 ppb or less
Regard a value of more than 20% variability as a positive test
- Consider monitoring peak flow variability for 2–4 weeks in adults (aged 17 and over) if there is diagnostic uncertainty after initial assessment and they have:
- obstructive spirometry and
- irreversible airways obstruction (negative BDR) and
- a FeNO level between 25 and 39 ppbRegard a value of more than 20% variability as a positive test
- Monitor peak flow variability for 2–4 weeks in children and young people (aged 5–16) if there is diagnostic uncertainty after initial assessment and a FeNO test and they have either:
- normal spirometry or
- obstructive spirometry, irreversible airways obstruction (negative BDR) and a FeNO level of 35 ppb or more
Regard a value of more than 20% variability as a positive test.
Airway Hyperreactivity Measures
Direct Bronchial Challenge Test with Histamine or Methacholine
- Offer a direct bronchial challenge test with histamine or methacholine[B] to adults (aged 17 and over) if there is diagnostic uncertainty after a normal spirometry and either a:
- FeNO level of 40 ppb or more and no variability in peak flow readings or
- FeNO level of 39 ppb or less with variability in peak flow readings
Regard a PC20 value of 8 mg/ml or less as a positive test
- Consider a direct bronchial challenge test with histamine or methacholine[B] in adults (aged 17 and over) with:
- obstructive spirometry without bronchodilator reversibility and
- a FeNO level between 25 and 39 ppb and
- no variability in peak flow readings (less than 20% variability over 2–4 weeks)
Regard a PC20 value of 8 mg/ml or less as a positive test
- If a direct bronchial challenge test with histamine or methacholine is unavailable, suspect asthma and review the diagnosis after treatment, or refer to a centre with access to a histamine or methacholine challenge test.
Diagnosis in Children and Young People aged 5–16
See also Algorithm 2 for objective asthma assessment for children aged 5–16.- Diagnose asthma in children and young people (aged 5–16) if they have symptoms suggestive of asthma and:
- a FeNO level of 35 ppb or more and positive peak flow variability or
- obstructive spirometry and positive bronchodilator reversibility
- Suspect asthma in children and young people (aged 5–16) if they have symptoms suggestive of asthma and:
- a FeNO level of 35 ppb or more with normal spirometry and negative peak flow variability or
- a FeNO level of 35 ppb or more with obstructive spirometry but negative bronchodilator reversibility and no variability in peak flow readings or
- normal spirometry, a FeNO level of 34 ppb or less and positive peak flow variabilityDo not rule out other diagnoses if symptom control continues to remain poor after treatment. Review the diagnosis after 6 weeks by repeating any abnormal tests and reviewing symptoms.
- Refer children and young people (aged 5–16) for specialist assessment if they have obstructive spirometry, negative bronchodilator reversibility and a FeNO level of 34 ppb or less
- Consider alternative diagnoses and referral for specialist assessment in children and young people (aged 5–16) if they have symptoms suggestive of asthma but normal spirometry, a FeNO level of 34 ppb or less and negative peak flow variability.
Diagnosis in Adults aged 17 and Over
See also Algorithm 3 for objective tests in adults aged 17 and over.- Diagnose asthma in adults (aged 17 and over) if they have symptoms suggestive of asthma and:
- a FeNO level of 40 ppb or more with either positive bronchodilator reversibility or positive peak flow variability or bronchial hyperreactivity, or
- a FeNO level between 25 and 39 ppb and a positive bronchial challenge test, or
- positive bronchodilator reversibility and positive peak flow variability irrespective of FeNO level
- Suspect asthma in adults (aged 17 and over) with symptoms suggestive of asthma, obstructive spirometry and:
- negative bronchodilator reversibility, and either a FeNO level of 40 ppb or more, or a FeNO level between 25 and 39 ppb and positive peak flow variability, or
- positive bronchodilator reversibility, a FeNO level between 25 and 39 ppb and negative peak flow variability
Do not rule out other diagnoses if symptom control continues to remain poor after treatment. Review the diagnosis after 6–10 weeks by repeating spirometry and objective measures of asthma control and reviewing symptoms
- Consider alternative diagnoses, or referral for a second opinion, in adults (aged 17 and over) with symptoms suggestive of asthma and:
- a FeNO level below 40 ppb, normal spirometry and positive peak flow variability or
- a FeNO level of 40 ppb or more but normal spirometry, negative peak flow variability, and negative bronchial challenge test or
- obstructive spirometry with bronchodilator reversibility, but a FeNO level below 25 ppb, and negative peak flow variability or
- positive peak flow variability but normal spirometry, a FeNO level below 40 ppb, and a negative bronchial challenge test or
- obstructive spirometry with negative bronchodilator reversibility, a FeNO level below 25 ppb, and negative peak flow variability (if measured).
Diagnosis in People who are Unable to Perform an Objective Test
For young children who cannot perform objective tests, see the section Diagnosing asthma in young children.- If an adult, young person or child with symptoms suggestive of asthma cannot perform a particular test, try to perform at least two other objective tests. Diagnose suspected asthma based on symptoms and any positive objective test results.
Good Clinical Practice in Asthma Diagnosis
- Record the basis for a diagnosis of asthma in a single entry in the person’s medical records, alongside the coded diagnostic entry.
Diagnostic Summary
Table 1: Positive Test Thresholds for Objective Tests for Adults, Young People, and Children (Aged 5 and Over)
| Test | Population | Positive Result |
|---|---|---|
| FeNO | Adults | 40 ppb or more |
| Children and young people | 35 ppb or more | |
| Obstructive spirometry | Adults, young people, and children | FEV1/FVC ratio less than 70% (or below the lower limit of normal if this value is available) |
| BDR test | Adults | Improvement in FEV1 of 12% or more and increase in volume of 200 ml or more |
| Children and young people | Improvement in FEV1 of 12% or more | |
| Peak flow variability | Adults, young people, and children | Variability over 20% |
| Direct bronchial challenge test with histamine or methacholine | Adults | PC20 of 8 mg/ml or less |
| Children and young people | n/a | |
| Abbreviations: BDR=bronchodilator reversibility; FeNO=fractional exhaled nitric oxide; FEV1 =forced expiratory volume in 1 second; FVC=forced vital capacity; PC20 =provocative concentration of methacholine causing a 20% fall in FEV1 | ||
Monitoring Asthma Control
- Monitor asthma control at every review. If control is suboptimal:
- confirm the person’s adherence to prescribed treatment in line with the recommendations on assessing adherence in the NICE guideline on medicines adherence
- review the person’s inhaler technique
- review if treatment needs to be changed
- ask about occupational asthma and/or other triggers, if relevant
- Consider using a validated questionnaire (for example, the Asthma Control Questionnaire or Asthma Control Test) to monitor asthma control in adults (aged 17 and over)
- Monitor asthma control at each review in adults, young people and children aged 5 and over using either spirometry or peak flow variability testing
- Do not routinely use FeNO to monitor asthma control
- Consider FeNO measurement as an option to support asthma management in people who are symptomatic despite using inhaled corticosteroids. (This recommendation is from NICE’s diagnostics guidance on measuring fractional exhaled nitric oxide concentration in asthma)
- Do not use challenge testing to monitor asthma control.
- Observe and give advice on the person’s inhaler technique:
- at every consultation relating to an asthma attack, in all care settings
- when there is deterioration in asthma control
- when the inhaler device is changed
- at every annual review
- if the person asks for it to be checked.
Footnotes
[A] Apply the principles in the recommendation under Diagnosing asthma in young children for young children unable to do the FeNO test adequately
[B] At the time of publication (November 2017), the use of histamine and methacholine was off-label. See NICE’s information on prescribing medicines

