Overview
This Guidelines summary sets out an antimicrobial prescribing strategy for acute exacerbations of chronic obstructive pulmonary disease (COPD), including a useful algorithm for choosing an antibiotic.
Fluoroquinolone antibiotics: In January 2024, the Medicines and Healthcare products Regulatory Agency published a Drug Safety Update on fluoroquinolone antibiotics. These must now only be prescribed when other commonly recommended antibiotics are inappropriate.
Reflecting on your Learnings
Reflection is important for continuous learning and development, and a critical part of the revalidation process for UK healthcare professionals. Click here to access the Guidelines Reflection Record.
Algorithm 1: Antibiotics for COPD (Acute Exacerbation)
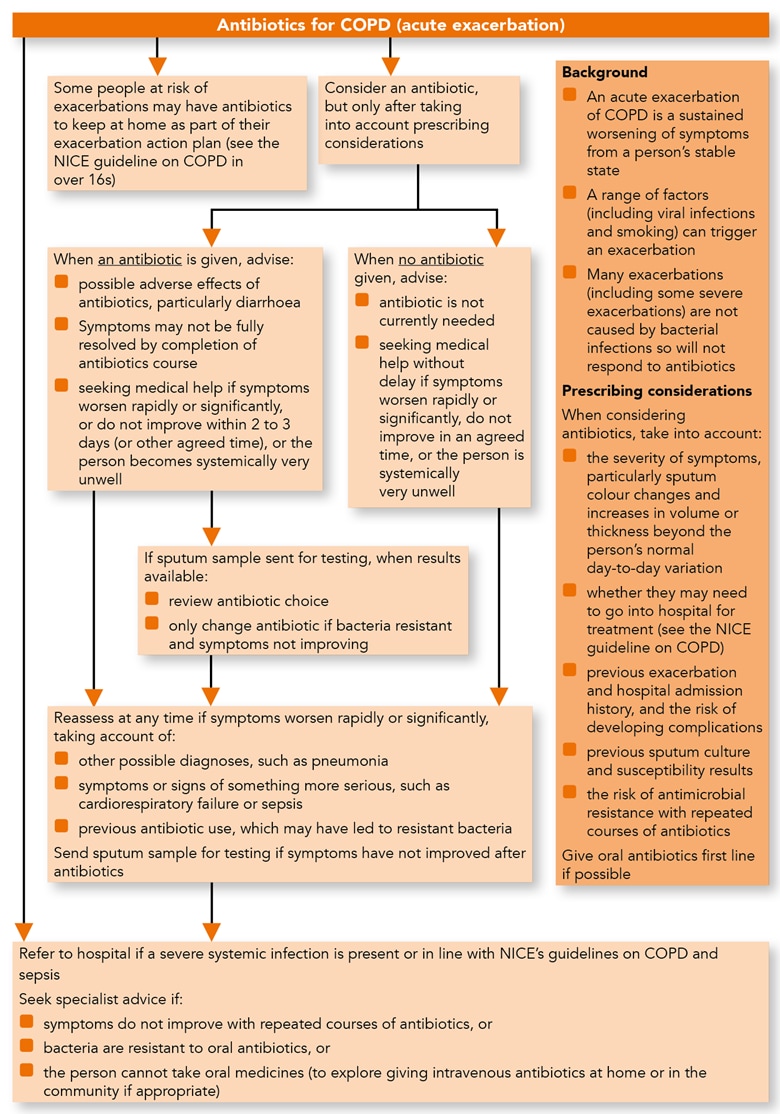
Managing an Acute Exacerbation of COPD with Antibiotics
- Be aware that:
- an acute exacerbation of chronic obstructive pulmonary disease (COPD) is a sustained worsening of symptoms from a person’s stable state
- a range of factors (including viral infections and smoking) can trigger an exacerbation
- many exacerbations (including some severe exacerbations) are not caused by bacterial infections so will not respond to antibiotics
- some people at risk of exacerbations may have antibiotics to keep at home as part of their exacerbation action plan (see the recommendations on choice of antibiotic).
See the NICE guideline on COPD in over 16s.
Treatment
- Consider an antibiotic (see the recommendations on choice of antibiotic) for people with an acute exacerbation of COPD, but only after taking into account:
- the severity of symptoms, particularly sputum colour changes and increases in volume or thickness beyond the person’s normal day-to-day variation
- whether they may need to go into hospital for treatment (see the NICE guideline on COPD in over 16s)
- previous exacerbation and hospital admission history, and the risk of developing complications
- previous sputum culture and susceptibility results
- the risk of antimicrobial resistance with repeated courses of antibiotics.
- If a sputum sample has been sent for culture and susceptibility testing (in line with the NICE guideline on COPD in over 16s) and an antibiotic has been given:
- review the choice of antibiotic when results are available and
- only change the antibiotic according to susceptibility results if bacteria are resistant and symptoms are not already improving (using a narrow-spectrum antibiotic wherever possible).
- If an antibiotic is given, give advice:
- about possible adverse effects of the antibiotic, particularly diarrhoea
- that symptoms may not be fully resolved when the antibiotic course has been completed
- about seeking medical help if:
- symptoms worsen rapidly or significantly or
- symptoms do not start to improve within 2–3 days (or other agreed time) or
- the person becomes systemically very unwell.
- If no antibiotic is given, give advice about:
- an antibiotic not being needed currently
- seeking medical help without delay if:
- symptoms (such as sputum colour changes and increases in volume or thickness) worsen rapidly or significantly or
- symptoms do not start to improve within an agreed time or
- the person becomes systemically very unwell.
Reassessment
- Reassess people with an acute exacerbation of COPD if their symptoms worsen rapidly or significantly at any time, taking account of:
- other possible diagnoses, such as pneumonia
- any symptoms or signs suggesting a more serious illness or condition, such as cardiorespiratory failure or sepsis
- previous antibiotic use, which may have led to resistant bacteria.
Send a sputum sample for culture and susceptibility testing if symptoms have not improved following antibiotic treatment and this has not been done already.
Referral and Seeking Specialist Advice
- Refer people with an acute exacerbation of COPD to hospital if they have any symptoms or signs suggesting a more serious illness or condition (for example, cardiorespiratory failure or sepsis) and in line with the NICE guideline on COPD in over 16s.
- Seek specialist advice for people with an acute exacerbation of COPD if they:
- have symptoms that are not improving with repeated courses of antibiotics or
- have bacteria that are resistant to oral antibiotics or
- cannot take oral medicines (to explore locally available options for giving intravenous antibiotics at home or in the community, rather than in hospital, where appropriate).
Choice of Antibiotic
- When prescribing an antibiotic for an acute exacerbation of COPD, follow table 1 for adults aged 18 years and over.
- Give oral antibiotics first line if the person can take oral medicines, and the severity of their exacerbation does not require intravenous antibiotics.
- Review intravenous antibiotics by 48 hours and consider stepping down to oral antibiotics where possible.
Table 1: Antibiotic Treatment for Adults Aged 18 Years and Over
| Antibiotic[A],[B] | Dosage and course length |
|---|---|
| First-choice oral antibiotics (empirical treatment or guided by most recent sputum culture and susceptibilities) | |
| Amoxicillin | 500 mg three times a day for 5 days (see BNF for dosage in severe infections) |
| Doxycycline | 200 mg on first day, then 100 mg once a day for 5‑day course in total (see BNF for dosage in severe infections) |
| Clarithromycin | 500 mg twice a day for 5 days |
| Second-choice oral antibiotics (no improvement in symptoms on first choice taken for at least 2 to 3 days; guided by susceptibilities when available) | |
| Use alternative first choice (from a different class) | as above |
| Alternative choice oral antibiotics (if person at higher risk of treatment failure;[C] guided by susceptibilities when available) | |
| Co-amoxiclav | 500/125 mg three times a day for 5 days |
| Co-trimoxazole[D] | 960 mg twice a day for 5 days |
| Levofloxacin (with specialist advice if co-amoxiclav or co-trimoxazole cannot be used; consider safety issues[E]) | 500 mg once a day for 5 days |
| First-choice intravenous antibiotic (if unable to take oral antibiotics or severely unwell; guided by susceptibilities when available)[F] | |
| Amoxicillin | 500 mg three times a day (see BNF for dosage in severe infections) |
| Co-amoxiclav | 1.2 g three times a day |
| Clarithromycin | 500 mg twice a day |
| Co-trimoxazole[D] | 960 mg twice a day (see BNF for dosage in severe infections) |
| Piperacillin with tazobactam | 4.5 g three times a day (see BNF for dosage in severe infections) |
| Second-choice intravenous antibiotic | |
| Consult local microbiologist; guided by susceptibilities | |
| [A] See the British national formulary (BNF) for appropriate use and dosing in specific populations, for example, hepatic impairment, renal impairment, and administering intravenous antibiotics. [B] If a person is receiving antibiotic prophylaxis, treatment should be with an antibiotic from a different class. [C] People who may be at a higher risk of treatment failure include people who have had repeated courses of antibiotics, a previous or current sputum culture with resistant bacteria, or people at higher risk of developing complications. [D] Co-trimoxazole should only be considered for use in acute exacerbations of COPD when there is bacteriological evidence of sensitivity and good reason to prefer this combination to a single antibiotic (BNF, October 2018). [E] See MHRA advice for restrictions and precautions for using fluoroquinolone antibiotics due to very rare reports of disabling and potentially long-lasting or irreversible side effects affecting musculoskeletal and nervous systems. Warnings include: stopping treatment at first signs of a serious adverse reaction (such as tendonitis), prescribing with special caution in people over 60 years and avoiding coadministration with a corticosteroid (March 2019). [F] Review intravenous antibiotics by 48 hours and consider stepping down to oral antibiotics where possible. [G] See the evidence and committee discussion on choice of antibiotic and antibiotic course length. | |

