Overview
This guideline was developed by a multiprofessional consensus panel with expertise and an interest in malnutrition and COPD, representing a number of professional associations. It has been endorsed by BAPEN, RCGP, RCN, ARNS, BDA, PCRS, ACPRC, NNNG, BLF and Education for Health. BAPEN, ARNS and the NNNG reviewed and approved the publication of this summary.
Identification of Malnutrition—Nutritional Screening
- Identifying and managing malnutrition (in the general population and in individuals with chronic obstructive pulmonary disease (COPD)) can improve nutritional status, clinical outcomes, and reduce healthcare use
- Routine nutritional risk screening with a validated screening tool should be performed in all COPD patients across all settings
- NICE guidelines recommend body mass index (BMI) is calculated in all patients with COPD and that attention should be paid to unintentional weight loss particularly in older people
- Screening should take place on first contact with a patient and/or upon clinical concern e.g. recent exacerbation, change in social or psychological status. A review should take place at least annually and more frequently if risk of malnutrition is identified
- It should be noted that BMI alone will not identify all patients who are at risk of malnutrition as a high BMI can mask unintentional weight loss including loss of muscle mass (lean tissue)
- NICE Guideline 115 (NG115) Chronic obstructive pulmonary disease in over 16s: diagnosis and management recommends attention is paid to changes in weight in older people, particularly if the change is more than 3 kg – such weight changes should however be taken within the context of the individuals original weight as a 3 kg weight loss in a 100 kg individual and a 45 kg individual is very different. Weight change should also be considered in terms of % change from usual weight e.g. 10% unplanned weight loss over 6 months, and in the context of time e.g. rapid daily changes can reflect fluid balance
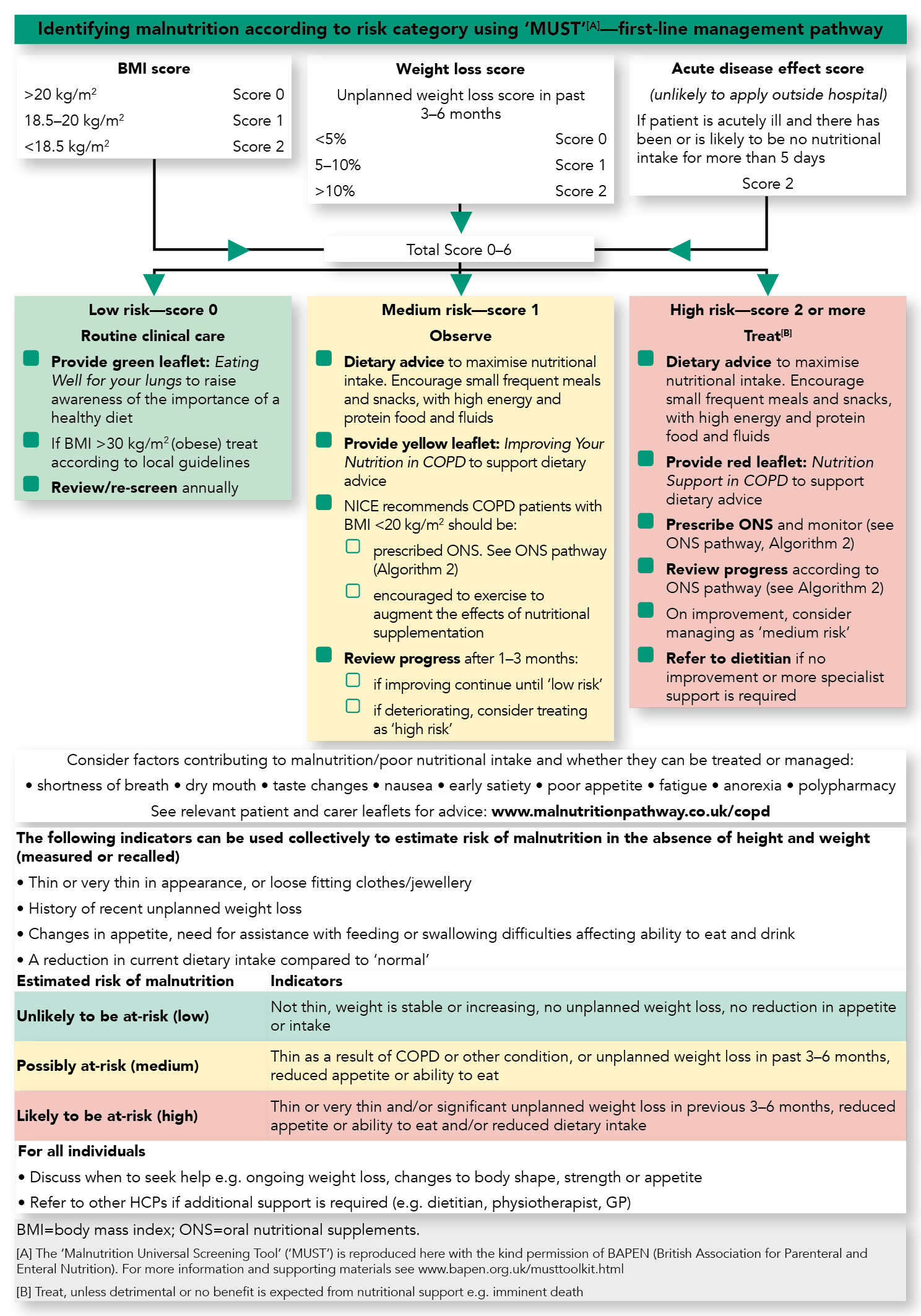
- The Malnutrition Universal Screening Tool (‘MUST’) is a simple 5-step screening tool that can be used across care settings to identify adults who are at risk of malnutrition (see Algorithm 1). It combines assessment of BMI, recent unplanned weight loss, and presence of acute illness:
- Unintentional weight loss of 5–10% over 3–6 months indicates risk of malnutrition irrespective of BMI
- ‘MUST’ is a predictor for risk of death and readmission in patients with COPD.
Considerations
- Weight loss may be a sign of other conditions, e.g. malignancy. Other conditions should therefore be considered and excluded before assuming the weight loss is COPD related. Nutritional advice can be instigated and should not be delayed whilst awaiting further investigations
- Care should be taken when interpreting BMI or percentage weight loss if oedema is present. Mid upper arm circumference (MUAC) can be used in the presence of severe oedema, or in the absence of weight measurement, to estimate BMI (MUAC of <23 cm often indicates a BMI <20 kg/m2) (See The ‘MUST’ explanatory booklet for further details)
- Hand grip strength may be used as a surrogate marker for muscle strength
- Depression and social isolation may be a problem in this group. Being housebound or having limited social activity can impact on ability to prepare and eat food.
Principles of the Management of Malnutrition in COPD
- Once identified as at risk of malnutrition, individuals with COPD can be managed using the pathways in this summary (see Algorithms 1 and 2). The principles of the management strategies in the pathways are detailed below
- Management of malnutrition should be linked to the risk category (low, medium, or high risk)
- For all individuals:
- record risk
- agree goals of intervention
- monitor.
Goal Setting—Agree Goals of Intervention with Individual/Carer
- Set goals to assess the effectiveness of intervention, taking into account the stage of the disease e.g. nutritional support for weight maintenance or weight gain
- Goals could include: increase lean body mass, improve nutritional status, improve respiratory function, stabilise weight and retain function. (NB: goals need to be adjusted according to phase of disease, patient centred and realistic e.g. in palliative care or advanced illness goals may include slowing rate of weight loss)
- Stable COPD: it may be appropriate to aim for an increase in body weight and muscle mass (lean tissue). Amongst those who are malnourished a 2 kg increase is suggested as a threshold at which functional improvements are seen; timescales to achieve weight gain will depend on the individual’s condition
- Acute exacerbations: minimising the loss of weight and muscle mass (lean tissue) through nutritional intervention may be an appropriate goal
- Pulmonary rehabilitation: is recommended as part of the management of individuals with COPD, and nutrition should be incorporated as part of the intervention
- nutritional intervention in patients with COPD at risk of malnutrition has been found to be associated with improved outcomes of exercise programmes
- dietary advice within programmes should be tailored to the individual e.g. for obese patients the goal may be weight reduction with preservation of muscle mass (lean tissue)
- consideration should be given to optimising nutritional status during pulmonary rehabilitation
- muscle protein is directly affected by protein intake in the diet and muscle oxidative metabolism may be stimulated nutritionally
- nutritional status should be monitored before, during and after pulmonary rehabilitation
Management of Malnutrition
- Follow guidance in the management pathway (see Algorithm 1). This includes different strategies depending on the malnutrition risk category
- Management options can include: dietary advice, assistance with eating, texture modified diets, and oral nutritional supplements (ONS) where indicated
- Dietary advice should aim to increase intake of all nutrients including energy, protein, and micronutrients (vitamins and minerals)
- Dietary advice and ONS should be considered for those at risk of malnutrition to ensure further weight loss is prevented and functional measures are improved (e.g. sit to stand and 6-minute walk test)
- Consideration should be given to issues which may impact on food intake and the practicalities of dietary advice, such as access to food, reduced mobility and breathlessness e.g. mMRC ≥2
- Smoking cessation is an important strategy to support the management of malnutrition and may increase appetite and support weight gain. Patients may also find their senses of smell and taste are enhanced if smoking is stopped, making food more pleasurable. Encourage smoking cessation to preserve lung function and improve appetite and taste.
Monitoring Progress
- Monitor progress against goals and modify intervention appropriately
- Consider weight change, hand-grip strength, sit to stand, along with observations including ability to perform activities of daily living, physical appearance, appetite and disease progression
- Frequency of monitoring depends on the risk category and intervention
- Further information on nutritional monitoring can be found in insert NICE Clinical Guideline 32 (CG32) Nutrition support for adults: oral nutrition support, enteral tube feeding, and parenteral nutrition.
Identifying Malnutrition Using 'MUST' Algorithm
Algorithm 1: Identifying Malnutrition According to Risk Category Using ‘MUST’[A]—First-line Management Pathway
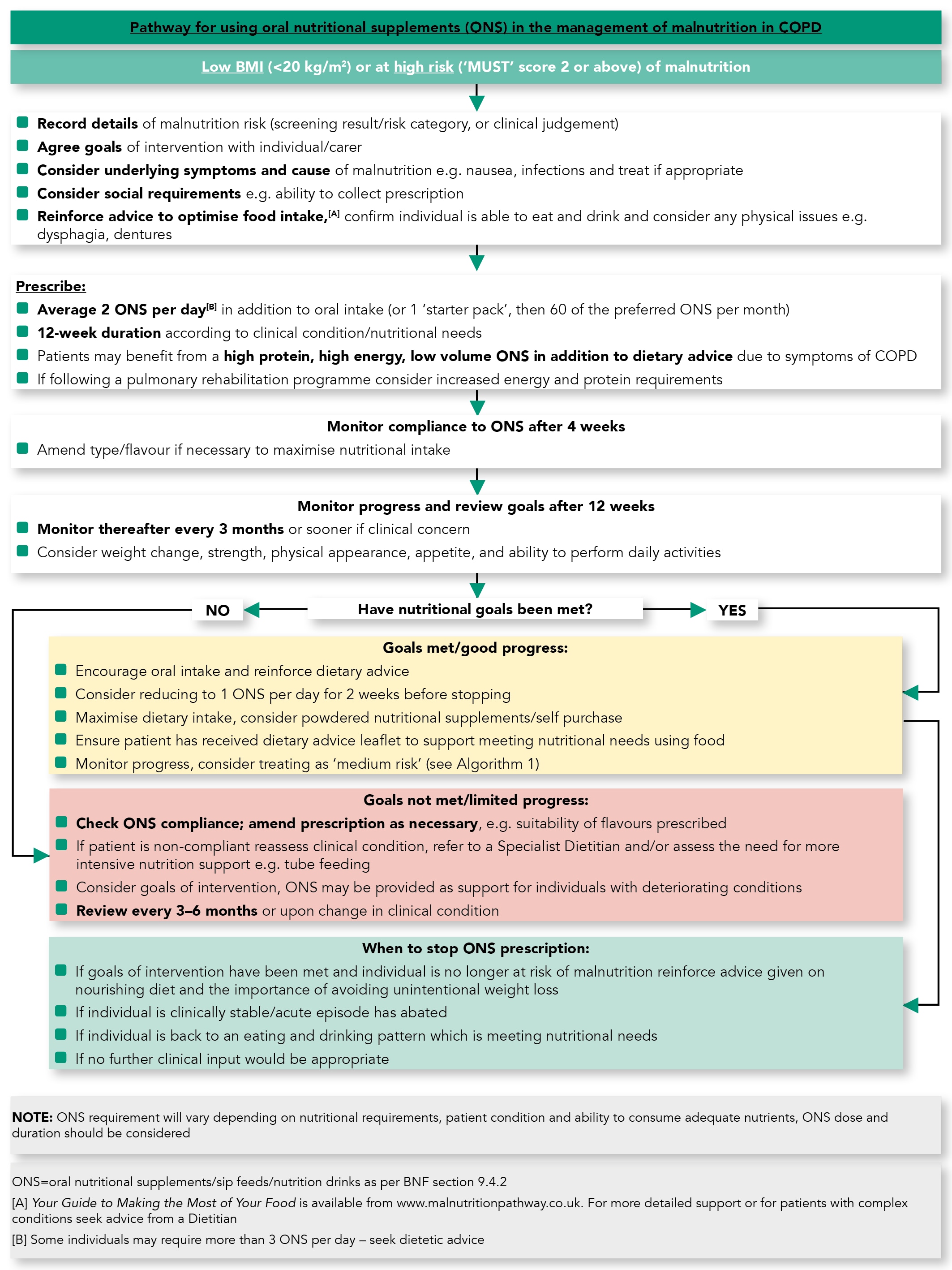
ONS Management Algorithm
Algorithm 2: Pathway for Using ONS in the Management of Malnutrition in COPD
Optimising Nutritional Intake
Optimising Nutritional Intake—An Evidence-based Approach to Managing Malnutrition
NICE Guidance (NG115 and CG32)
- NICE COPD guideline (NG115) Chronic obstructive pulmonary disease in over 16s: diagnosis and management recommends ONS are provided for individuals with COPD with a low BMI (<20 kg/m2). Further information on oral nutrition support is available in NICE Clinical Guideline 32 (CG32) Nutrition support for adults: oral nutrition support, enteral tube feeding and parenteral nutrition.
Dietary Advice to Optimise Nutritional Intake
- Dietary advice in malnourished patients with COPD should be used with care to ensure that requirements for all essential nutrients i.e. energy, protein, vitamins and minerals, are met or given due consideration
- Energy and protein requirements are likely to be higher or increased for patients who are:
- at nutritional risk/moderately or severely malnourished
- acutely unwell/have an infection
- exercising where accrual of muscle mass is the aim(See the PENG guidelines for further information)
- The amount of protein recommended in those with COPD is estimated as follows:
- 0.8 - 1.5 g protein/kg of body weight/day for non-malnourished/not at nutritional risk/stable COPD
- up to 1.5 g protein/kg of body weight/day in acutely unwell (exacerbating) patients where the aim is to meet requirements/attenuate further losses
- where the goal is to gain or retain lean mass, in conjunction with exercise (e.g. pulmonary rehabilitation) and/ or in malnourished outpatients where weight gain is the goal, it is possible up to 1.5 g protein/kg of body weight/day may be required (NB: in obese or overweight patients protein requirements should be calculated on ideal body weight)
- in the absence of being able to translate the above requirements into amounts of protein required by an individual, patients should be encouraged to eat 3-4 portions of high protein foods per day – for further information/ideas on protein see www.malnutritionpathway.co.uk/proteinfoods
- Patients with COPD are at high risk of osteoporosis if they require frequent steroid therapy, are inactive and/or have little exposure to sunlight e.g. are housebound. Attention should be given to addressing requirements for vitamin D and calcium including the need for supplementation
- Dietary advice should be an integral part of COPD management across the continuum of care, this core document is therefore supported by a range of patient advice leaflets (red, yellow, green) which have been designed to help provide practical nutritional advice to patients according to nutritional status, nutritional risk and disease status – www.malnutritionpathway.co.uk/copd
- Individuals with COPD may have concerns which affect the acceptability of dietary advice e.g. reservations about weight gain. Patient-centred discussions should be undertaken to discuss the potential benefit of nutritional interventions e.g. to maintain lung strength, overcome infection, improve ability to perform activities of daily living
- Consideration should be given to the patient/carer’s ability to act on the dietary advice given, with regular monitoring built into clinical reviews.
ONS to Optimise Nutritional Intake
- Dietary advice forms an important component of the management pathway, and should be used alongside ONS where indicated, i.e. where BMI is low (<20 kg/m2) or in high risk individuals (unintentional weight loss >10% over 3–6 months)
- Evidence from systematic reviews show that ONS in addition to diet in COPD can:
- significantly improve hand-grip strength
- significantly improve respiratory muscle strength
- enhance exercise performance
- significantly improve patients’ nutritional intake
- significantly improve weight
- improve quality of life
- ONS increase total nutrient intakes (energy, protein and micronutrients) without affecting dietary intake
- Higher energy ONS (≥2 kcal/ml) or low volume, high energy ONS (125 ml) may aid compliance and be easier to manage for individuals with early satiety and/or breathlessness
- Increased requirements for protein and other nutrients in COPD may be managed with a high protein, high energy, low volume ONS
- Low volume, energy dense ONS to be taken in small, frequent doses e.g. between meals (frequent small amounts of ONS are preferred to avoid postprandial dyspnoea and satiety as well as to improve compliance)
- Clinical benefits of ONS are often seen with 300–900 kcal/day (average 2 bottles), typically within 2–3 months of supplementation
- The exact choice of ONS should be based on a detailed nutritional assessment and patient preferences, and be in line with the recommendation to achieve an additional intake in the region of ~600 kcal/day.
In all patients, care should be taken to ensure advice on adequate hydration is given.

