One airway disease
Allergic rhinitis (AR) is a common comorbidity in >80% of patients with asthma but is frequently undertreated and underdiagnosed[3,7]
AR is an independent risk factor for developing asthma, and increases the risk of a patient’s asthma being poorly controlled[1]
Treating AR can improve patient’s asthma symptoms and reduce the odds of asthma-related emergency department visits and hospitalisations[7]
Respiratory symptoms thought to be caused by asthma (coughing, wheezing, and breathlessness) may sometimes be solely caused by AR.
Top tips for patients
Seasonal AR
Allergens are usually tree pollen (spring), grass pollen (end of spring/beginning of summer), or weeds (early spring to late autumn)[3]
Allergen avoidance strategies can help reduce symptoms, such as minimising outdoor activity, wearing wraparound sunglasses, shutting windows in cars and buildings, using nasal filters, avoiding drying clothes outside when the pollen count is high, and showering and washing hair after pollen exposure[3,4]
Patients should start using treatment two weeks before they normally experience symptoms and stop at the end of the season.[4]
The Met Office pollen forecast (for the UK) can help with timings of when there is high to very high pollen count (see useful resources)
Pollen food syndrome affects some people with hay fever. Symptoms of itching and/or swelling of the lips, tongue, and mouth and/or throat may be experienced on eating some fruits, vegetables, or nuts, such as apples, because of the cross-reactivity between these foods and pollens, such as birch tree pollen.[3,8]
Non-pharmacological interventions
Nasal douching with saline may help reduce the severity of symptoms[3,4,9]
Allergen barrier balms that are applied around the nostrils may reduce the amount of pollen entering the airways and may reduce symptoms.[4,10]
Medication
Explain that treatment will be trialled for two to four weeks to enable diagnosis and assess its effectiveness, but a change in medication or referral may be required on review[3]
Advise patients when to expect improvement in symptoms:
intranasal corticosteroids can take 6–8 hours to begin working and around two weeks to achieve maximal effect[1,3,4]
intranasal antihistamines (AH) (azelastine hydrochloride) have a fast onset of action (15 minutes)[3,4]
combination azelastine hydrochloride and fluticasone propionate spray clinically improves symptoms days earlier than monotherapy[2,4,11]
Explain that treatment is only effective if taken every day as directed
Teach patients how to use nasal sprays correctly (see useful resources) and check their technique at each review
Warn patients about possible side effects – some patients may experience a bitter taste with azelastine, and epistaxis is a possibility with intranasal steroids.[4]
Considerations for healthcare professionals
Diagnosis
Questions about AR symptoms should be phrased according to the patient’s level of understanding and linguistic ability
Check which medicines patients have tried previously and whether any were effective[4]
Remember to check patients with AR for asthma symptoms.[1]
Medication
Patients should not use sedating oral AH, for example, chlorphenamine, hydroxyzine, and promethazine[2,4]
Intranasal AH are more effective at treating AR symptoms than oral AH[2,4]
Intranasal steroids are more effective than intranasal AH and also reduce nasal congestion[2,4]
Intranasal steroids with the lowest systemic bioavailability should be used to reduce the risk of systemic effects (mometasone furoate, fluticasone furoate, and fluticasone propionate)[1,4]
Combination therapy using an intranasal steroid and intranasal AH spray is more effective than monotherapy[2,4]
Concordance with treatment may be improved by using a simple treatment regimen, such as once-daily treatments or a single device[3,4]
In exceptional circumstances (for example, the patient’s wedding day), it may be appropriate to use a short course of oral prednisoloneC to rapidly alleviate symptoms[3]
Injectable steroids (for example, triamcinolone acetonide) should not be used for AR because of a poor risk–benefit profile.[4]
Monitoring/review
A visual analogue scale is a simple scoring system to measure AR symptoms (0 to 10) and show improvement, which can help improve patient concordance with treatment and achieve optimum control[2]
Where possible, patients can use the MASK–air app to record daily symptoms, enabling a simple treatment decision after two to four weeks trial of treatment based on changes to the patient’s score[2]
The two to four week review can be carried out by phone, email, or video consultation[2]
Check patient’s asthma symptoms at review. If they improve with successful AR treatment, asthma medications might need stepping down and monitoring.[3,4]
Children
Mometasone is licensed for use in children ≥3 years[3]
Combination intranasal steroid and intranasal antihistamine treatment is not licensed in children under 12 years.[11]
C: Not currently recommended due to COVID-19.
Useful resources
How to use nasal spray: www.asthma.org.uk/advice/inhaler-videos/nasal-spray/
BSACI. How to apply a nasal spray: www.bsaci.org/wp-content/uploads/2019/12/Howtouseanasalspray.pdf
How to do nasal douching: www.youtube.com/watch?v=GW2PiOFhFtY
BSACI. Nasal douching: www.bsaci.org/wp-content/uploads/2019/12/Howtoperformnasaldouching.pdf
Allergy UK factsheet on hay fever: www.allergyuk.org/information-and-advice/conditions-and-symptoms/11-hay-fever-allergic-rhinitis
MASK-air app: www.mask-air.com/
Met Office pollen count: www.metoffice.gov.uk/weather/warnings-and-advice/seasonal-advice/pollen-forecast
Date of preparation: July 2020
Download
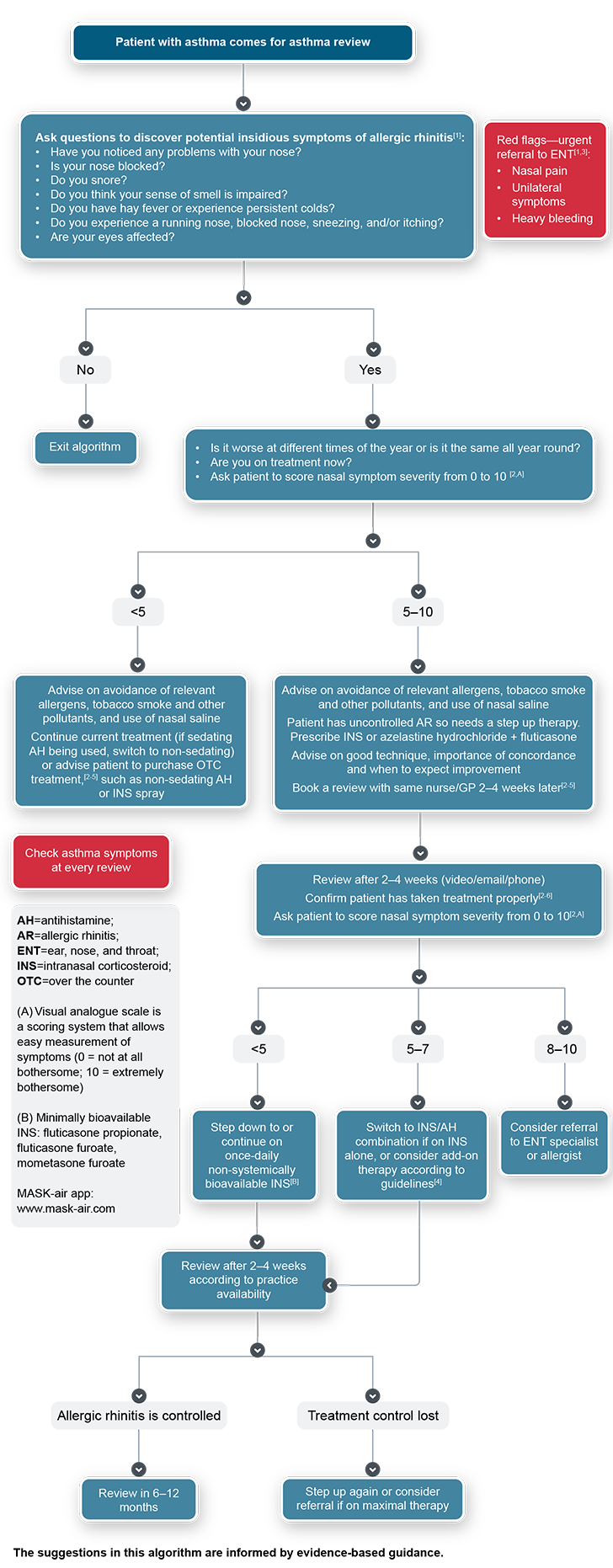
Algorithm: Identifying and managing allergic rhinitis in the asthma population
Credits:
Lead Image: denis_vermenko/stock.adobe.com
Medscape © 2020 WebMD, LLC
Any views expressed above are the author's own and do not necessarily reflect the views of WebMD or Medscape.
Cite this: Identifying and Managing Allergic Rhinitis in the Asthma Population - Medscape - Aug 17, 2020.







Comments