Overview
This Guidelines summary provides recommendations on the management of people with bronchiectasis in a primary care setting.
The British Thoracic Society (BTS) guideline for non-cystic fibrosis bronchiectasis, covering adults and children, was published in 2010 and updated in 2013. The new 2018 guideline covers bronchiectasis in adults and provides recommendations and good practice points based on an updated evidence review.
This summary is based on a 2019 summative paper by Gruffydd-Jones et al, which provides the relevant considerations from the full BTS guideline for primary care practitioners.
Initial Presentation of Bronchiectasis
- A diagnosis of bronchiectasis should be suspected when a patient presents with a recurrent or persistent (more than 8 weeks) cough with production of purulent or mucopurulent sputum, particularly with the relevant associated risk factors, such as chronic obstructive pulmonary disease (COPD)
- This diagnosis is particularly likely if the patient has a history of two or more COPD exacerbations per year and a previous positive sputum sample for Pseudomonas aeruginosa while stable (that is, not during an exacerbation)
- In addition to coincident presentation with COPD, a diagnosis of bronchiectasis should be suspected in patients presenting with persistent cough who also report difficult-to-treat asthma, rheumatoid arthritis, inflammatory bowel disease (IBD), chronic rhinosinusitis, or the presence of persistent sputum pathogens, especially P. aeruginosa.
History, Examination, and Investigations
- If bronchiectasis is suspected in a patient in a primary care setting, a full medical history and examination should be first directed to exclude other causes of cough, such as COPD, lung cancer, asthma, and gastro-oesophageal reflux
- Persistent basal, coarse lung crackles may be present
- Investigations in the primary care setting should encompass:
- diagnostic spirometry to look for other/coexistent diagnoses (such as COPD), and may be normal, restrictive, or obstructive
- sputum microbiology is helpful in identifying the presence of persistent pathogens, especially P. aeruginosa (indicating a worse prognosis)
- a chest X-ray should be carried out to help exclude alternative diagnoses, but has limited sensitivity for diagnosing bronchiectasis, especially in mild disease
- definitive diagnosis of bronchiectasis is made using thin-section computerised tomography (CT) scanning of the chest. It is highly accurate and diagnostic for bronchiectasis, with false-positive and false-negative rates of 1% and 2%, respectively
- referral for CT will usually be made via a secondary care specialist, although some primary care practitioners may have direct access
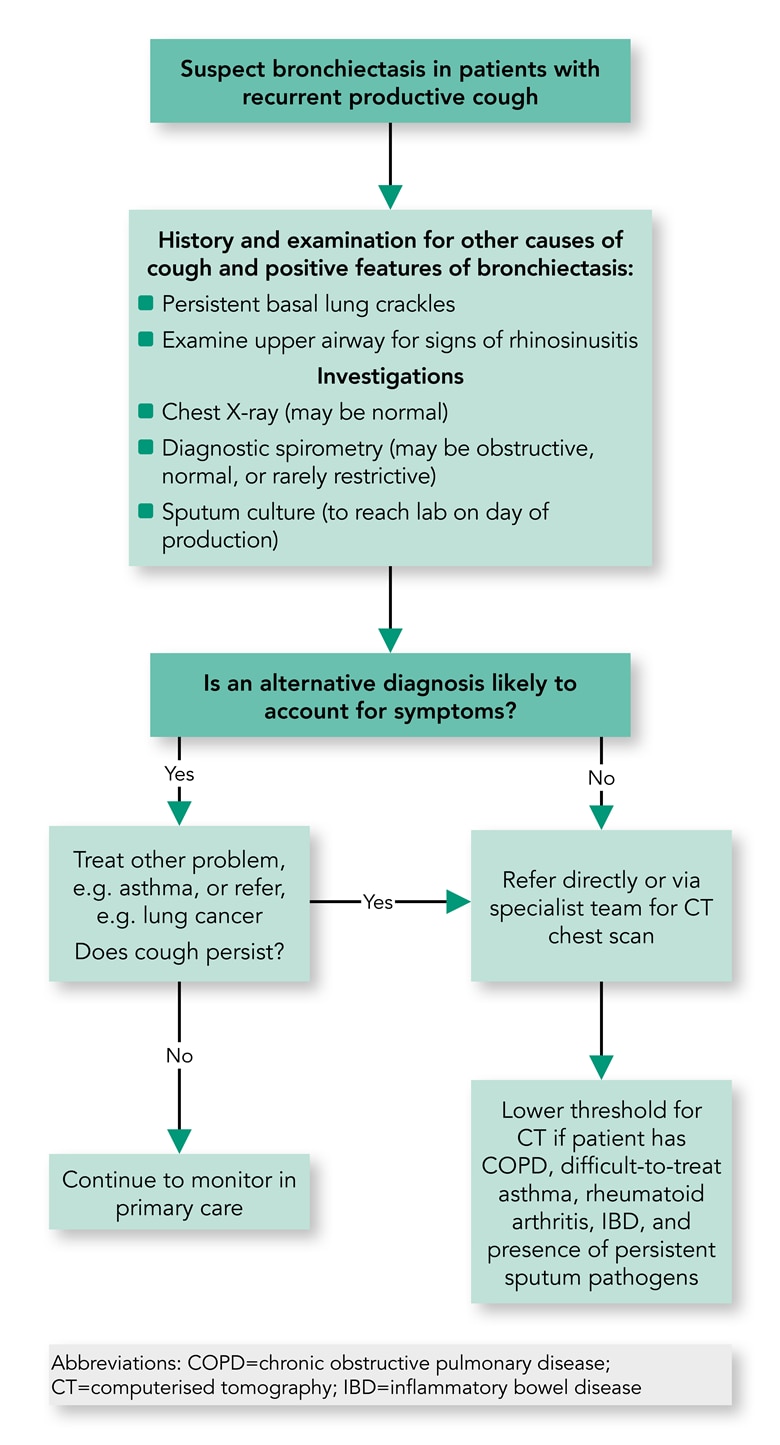
- Algorithm 1 shows a suggested diagnostic algorithm for patients suspected of having bronchiectasis in primary care.
Algorithm 1: Proposed Algorithm for the Diagnostic Pathway in Primary Care of Patients Suspected of Having Bronchiectasis
Assessment and Routine
- It is recommended that the initial assessment after diagnosis of bronchiectasis is carried out by a specialist respiratory team, where investigations can take place to elucidate any underlying cause and to formulate a treatment plan, which can be shared with the patient, primary care team, and community team where appropriate
- Comorbid conditions should be assessed, including asthma, COPD, gastro-oesophageal reflux disease, rheumatoid arthritis, and IBD, and treated accordingly
- The treatment plan should give details of treatment in the stable condition, advice on treatment in the event of an acute exacerbation, and arrangements for follow-up (primary care, hospital care, and shared care)
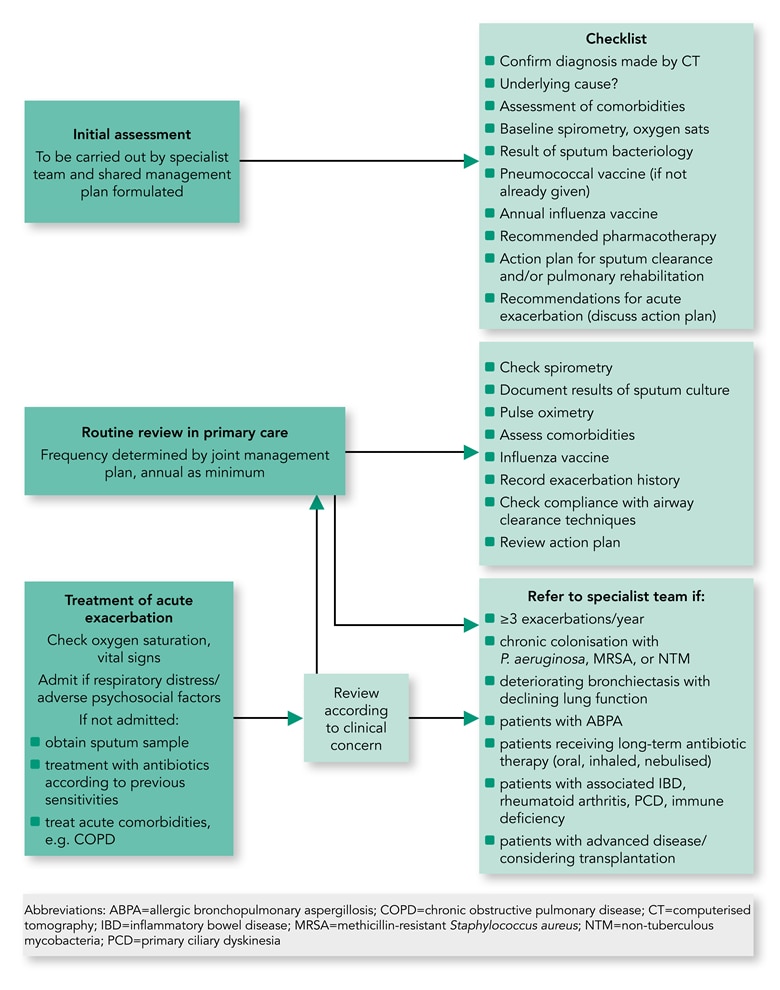
- See Algorithm 2 for a suggested checklist as part of the algorithm for review and management of patients with bronchiectasis in primary care.
Algorithm 2: Proposed Algorithm for the Review and Management of Patients With Bronchiectasis in Primary Care
Routine Review
- Patients at higher risk of future exacerbations should be reviewed in specialist care, where they present with or develop one or more of the following clinical situations:
- they experience three or more exacerbations in 1 year
- they have chronic P. aeruginosa, non-tuberculous mycobacteria, or methicillin-resistant Staphylococcus aureus colonisation
- there is deteriorating bronchiectasis with declining lung function
- they have associated rheumatoid arthritis, immune deficiency, IBD, or primary ciliary dyskinesia
- they have allergic bronchopulmonary aspergillosis
- patients with advanced disease and those considering lung transplantation
- Lower-risk patients can be routinely reviewed in primary care
- The exact frequency of review should be determined in the initial treatment plan, in consultation with the respiratory specialist, and also by changing clinical conditions, but should be at a minimum frequency of once a year.
- Factors to be routinely monitored by the primary care team (see Algorithm 2) include:
- assessment of symptoms (cough, sputum production, and breathlessness) and their impact on daily activities
- chronic cough that can have a significant effect on daily activities, including sexual relations and urinary incontinence in women
- exacerbation frequency
- body mass index (BMI)
- pulse oximetry
- spirometry
- the sputum should be sent for microbiological analysis when the patient is clinically stable, and should be sent at the start of an exacerbation before antibiotic treatment is started
- compliance with sputum clearance exercises and shared treatment plan
- Deterioration in lung function, exacerbation frequency, or clinical state should prompt specialist referral (see above)
- If the patient’s BMI is less than 20 kg/m2, then specialist nutritional advice should be sought
- The patient should be referred to a respiratory physiotherapist to reinforce the sputum clearance exercises if necessary
- Similarly, referral for pulmonary rehabilitation should be considered if the patient has functionally disabling breathlessness (Medical Research Council score of 2 or greater)
- Common comorbidities, such as mild-to-moderate asthma or COPD, can be treated in the primary care setting according to national or international guidelines for these conditions. It is recommended that chronic rhinosinusitis be treated with nasal saline douching and intranasal steroids.
Management
- The overall aims of management are to prevent further damage (treat the underlying cause if possible), maximise function and quality of life, and prevent and treat exacerbations
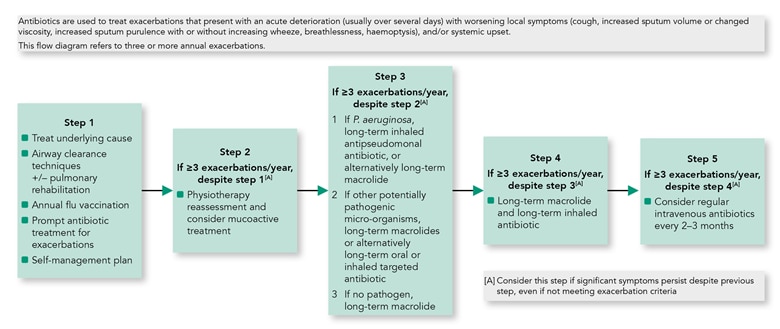
- Algorithm 3 shows a stepwise approach to management.
Algorithm 3: Stepwise Management of Patients with Bronchiectasis
Flu and Pneumococcal Immunisation
- It is important to offer annual flu immunisation to all patients with bronchiectasis
- The BTS recommends that polysaccharide pneumococcal vaccination should be offered to all patients with bronchiectasis (if not previously given).
Inhaled Corticosteroids and Bronchodilators
- Treatment with inhaled corticosteroids in bronchiectasis is not recommended, unless the drug is needed for comorbid diseases, such as asthma or COPD, according to treatment guidelines
- It is recommended to offer a trial of long-acting inhaled bronchodilators in patients with significant breathlessness, or where there is coexistent asthma and/or COPD
- Use of long-acting beta2 agonists and long-acting anti-muscarinic agents is recommended in patients with significant breathlessness and coexistent obstructive airway disease of whatever aetiology.
Management of the Acute Exacerbation
- Where an acute exacerbation incident is suspected, the first step should be to assess the vital signs (pulse oximetry, pulse rate, respiratory rate, temperature, and blood pressure)
- In the primary care setting, the patient should be treated for acute comorbidities, such as asthma and COPD, according to disease-specific guidelines
- The patient should be considered for admission to a secondary care setting where:
- there are features of sepsis or respiratory distress
- there are significant comorbidities and/or psychosocial factors
- there is a need for intravenous antibiotics, where a community service to provide these is not available.
Acute Antibiotic Therapy
- Where possible, the sputum should be obtained for culture and sensitivity testing prior to commencing antibiotics. However, empirical antibiotics can be started while awaiting the sputum results
- Table 1 shows common organisms associated with acute exacerbations of bronchiectasis and their treatment in primary care
- In general, antibiotic courses for 14 days are standard and should always be used in patients infected with P. aeruginosa
- Shorter courses may suffice in patients with mild bronchiectasis (usually 7–10 days)
- It is recommended to consider providing a home sputum pot and standby antibiotics for future exacerbations.
Table 1: Common Organisms Associated with Acute Exacerbations of Bronchiectasis and Suggested Oral Antibiotics
| Organism | Recommended First-line Treatment | Length of Treatment | Recommended Second-line Treatment | Length of Treatment | |||
|---|---|---|---|---|---|---|---|
| Streptococcus pneumoniae | Amoxicillin 500 mg TDS | 14 days | Doxycycline 100 mg BD | 14 days | |||
| Haemophilus influenzae—beta lactamase negative | Amoxicillin 500 mg TDS or amoxicillin 1 g TDS or amoxicillin3 g BD | 14 days | Doxycycline 100 mg BD or ciprofloxacin 500 or 750 mg BD or ceftriaxone 2 g OD (IV) | 14 days | |||
| Haemophilus influenzae—beta lactamase positive | Amoxicillin with clavulanic acid 625 one tablet TDS | 14 days | Doxycycline 100 mg BD or ciprofloxacin 500 or 750 mg BD or ceftriaxone 2 g OD (IV) | 14 days | |||
| Moraxella catarrhalis | Amoxicillin with clavulanic acid 625 one tablet TDS | 14 days | Clarithromycin 500 mg BD or doxycycline 100 mg BD or ciprofloxacin 500 or 750 mg BD | 14 days | |||
| Staphylococcus aureus (methicillin sensitive) | Flucloxacillin 500 mg QDS | 14 days | Clarithromycin 500 mg BD or doxycycline 100 mg BD or amoxicillin with clavulanic acid 625 one tablet TDS | 14 days | |||
| Pseudomonas aeruginosa | Oral ciprofloxacin 500 mg BD (750 mg BD in more severe infection) | 14 days | Discuss with a respiratory specialist/microbiologist | ||||
| Abbreviations: BD=twice a day; IV=intravenous; OD=once a day; QDS=four times a day; TDS=three times a day | |||||||
Prognosis
- Patients with mild bronchiectasis should have a normal life expectancy, but in patients with more advanced bronchiectasis, there is an increased risk of recurrent exacerbations, vascular disease, and mortality.
For recommendations on physiotherapy and long-term antibiotic therapy, refer to the full summative article. For recommendations for secondary and tertiary care, refer to the full guideline.

