Overview
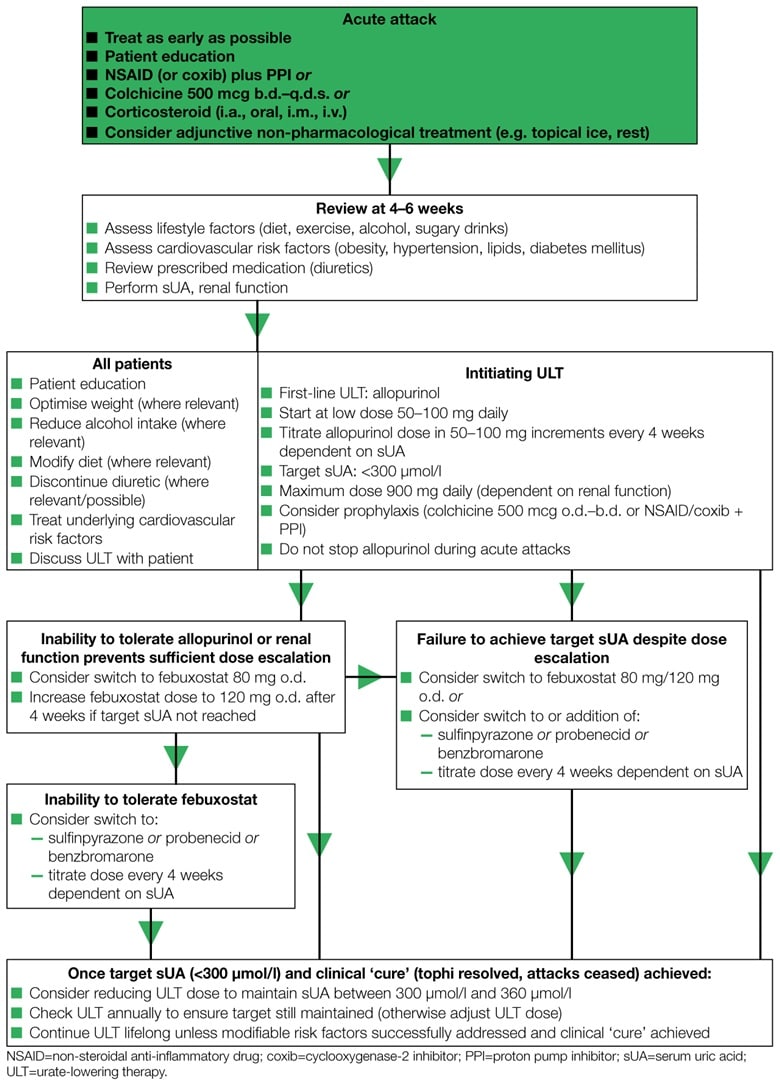
This summary of the British Society for Rheumatology's guideline on the management of gout covers risk factors, optimal use of ULTs, and management of acute attacks in primary care. It also includes a useful and concise management algorithm.
Reflecting on Your Learnings
Reflection is important for continuous learning and development, and a critical part of the revalidation process for UK healthcare professionals. Click here to access the Guidelines Reflection Record.
Background to the Disease
- Gout is the most common cause of inflammatory arthritis worldwide
- Clinical manifestations of gout resulting from monosodium urate crystal deposition include tophi, chronic arthritis, urolithiasis and renal disease as well as recurrent acute arthritis, bursitis and cellulitis
- Gouty arthritis and tophi are associated with chronic disability, impairment of health-related quality of life, increased use of healthcare resources and reduced productivity
- Gout is also frequently associated with co-morbidities such as obesity, dyslipidaemia, diabetes mellitus, chronic renal insufficiency, hypertension, cardiovascular disease, hypothyroidism, anaemia, psoriasis, chronic pulmonary diseases, depression and osteoarthritis as well as with an increase in all-cause mortality and urogenital malignancy
- Sustained hyperuricaemia is the single most important risk factor for the development of gout. Hyperuricaemia occurs secondarily to reduced fractional clearance of uric acid in >90% of patients with gout
- Age, male gender, menopausal status in females, impairment of renal function, hypertension and the co-morbidities that comprise the metabolic syndrome are all risk factors for incident gout associated with decreased excretion of uric acid, as are the use of diuretic and many anti-hypertensive drugs, ciclosporin, low-dose aspirin, alcohol consumption and lead exposure
- Tophi and chronic arthritis, alcohol consumption and recent use of diuretic drugs are important risk factors for recurring flares
Management of Acute Attacks
- Educate patients to understand that attacks should be treated as soon as an attack occurs and ensure that patients are aware of the importance of continuing any established urate-lowering therapy (ULT) during an attack
- Affected joints should be rested, elevated and exposed in a cool environment. Bed-cages and ice-packs can be effective adjuncts to management
- A non-steroidal anti-inflammatory drug (NSAID) at maximum dose or colchicine in doses of 500 mcg b.d.–q.d.s. is the drug of choice when there are no contraindications. Choice of first-line agent will depend on patient preference, renal function and co-morbidities. Patients on NSAIDs or cyclooxygenase-2 inhibitors (coxibs) should be co-prescribed a gastro-protective agent
- Joint aspiration and injection of a corticosteroid are highly effective in acute monoarticular gout and may be the treatment of choice in patients with acute illness and co-morbidity. A short course of oral corticosteroid or a single injection of an intramuscular corticosteroid is an alternative in patients who are unable to tolerate NSAIDs/colchicine and in whom intra-articular injection is not feasible. Such systemic therapy is also appropriate for oligo or polyarticular attacks of gout
- In patients with acute gout where response to monotherapy is insufficient, combinations of treatment can be used
- Interleukin-1 (IL-1) inhibitors may be considered in patients who have previously not responded adequately to standard treatment of acute gout (although not approved by the National Institute for Health and Care Excellence [NICE])
Modification of Lifestyle and Risk Factors
- If diuretic drugs are being used to treat hypertension rather than heart failure, an alternative antihypertensive agent can be considered as long as blood pressure is controlled
- All patients with gout should be given verbal and written information about the following: the causes and consequences of gout and hyperuricaemia; how to manage acute attacks; lifestyle advice about diet, alcohol consumption and obesity; and the rationale, aims and use of ULT to target urate levels. Management should be individualized and take into account co-morbidities and concurrent medications. Illness perceptions and potential barriers to care should be discussed
- In overweight patients, dietary modification to achieve a gradual reduction in body weight and subsequent maintenance should be encouraged. Diet and exercise should be discussed with all patients with gout, and a well-balanced diet low in fat and added sugars, and high in vegetables and fibre should be encouraged: sugar-sweetened soft drinks containing fructose should be avoided; excessive intake of alcoholic drinks and high purine foods should be avoided; and inclusion of skimmed milk and/or low fat yoghurt, soy beans and vegetable sources of protein, and cherries in the diet should be encouraged
- Patients with gout and a history of urolithiasis should be encouraged to drink >2 l of water daily and avoid dehydration. Alkalinization of the urine with potassium citrate (60 mEq/day) should be considered in recurrent stone formers
- Cardiovascular risk factors and co-morbid conditions such as cigarette smoking, hypertension, diabetes mellitus, dyslipidaemia, obesity and renal disease should be screened for in all patients with gout, reviewed at least annually and managed appropriately
Algorithm for the Management of Gout
Algorithm 1: Management of Gout
Optimal Use of Urate-lowering Therapies
- The option of ULT should be explained to patients when the diagnosis is confirmed and they are being given information about gout. Patients should be fully involved in the decision as to when to commence ULT. The importance of taking ULT regularly and continually to prevent the return of gout attacks should be explained. Patients should be supported during the process of lowering their serum uric acid levels as it can cause an increase in gout flares during this time
- ULT should be discussed and offered to all patients who have a diagnosis of gout. ULT should particularly be advised in patients with the following: recurring attacks (≥2 attacks in 12 months); tophi; chronic gouty arthritis; joint damage; renal impairment (estimated glomerular filtration rate [eGFR] <60 ml/min); a history of urolithiasis; diuretic therapy use; and primary gout starting at a young age
- Commencement of ULT is best delayed until inflammation has settled as ULT is better discussed when the patient is not in pain
- The initial aim of ULT is to reduce and maintain the sUA level at or below a target level of 300 µmol/l to prevent further urate crystal formation and to dissolve away existing crystals. The lower the sUA the greater the velocity of crystal elimination. After some years of successful treatment, when tophi have resolved and the patient remains free of symptoms, the dose of ULT can be adjusted to maintain the sUA at or below a less stringent target of 360 µmol/l to avoid further crystal deposition and the possibility of adverse effects that may be associated with a very low sUA
- Allopurinol is the recommended first-line ULT to consider. It should be started at a low dose (50–100 mg daily) and the dose then increased in 100 mg increments approximately every 4 weeks until the sUA target has been achieved (maximum dose 900 mg)
- In patients with renal impairment, smaller increments (50 mg) should be used and the maximum dose will be lower, but target urate levels should be the same
- Febuxostat can be used as an alternative second-line xanthine oxidase inhibitor for patients in whom allopurinol is not tolerated or whose renal impairment prevents allopurinol dose escalation sufficient to achieve the therapeutic target. Start with a dose of 80 mg daily and, if necessary, increase after 4 weeks to 120 mg daily, to achieve therapeutic target
- Uricosuric agents can be used in patients who are resistant to, or intolerant of, xanthine oxidase inhibitors. The preferred drugs are sulfinpyrazone (200–800 mg/day) or probenecid ( 500–2000 mg/ day) in patients with normal or mildly impaired renal function, or benzbromarone (50–200 mg/day) in patients with mild to moderate renal insufficiency
- Losartan and fenofibrate should not be used as a primary ULT but where treatment for hypertension or dyslipidaemia, respectively, is required, they may be considered as they have a weak uricosuric effect. Vitamin C supplements (500–1500 mg daily) also have a weak uricosuric effect
- A uricosuric agent can be used in combination with a xanthine oxidase inhibitor in patients who do not achieve a therapeutic serum urate target with optimal doses of monotherapy
- Colchicine 500 mcg b.d. or o.d. should be considered as prophylaxis against acute attacks resulting from initiation or up-titration of any ULT and continued for up to 6 months. In patients who cannot tolerate colchicine, a low-dose NSAID or coxib, with gastroprotection, can be used as an alternative providing there are no contraindications

