Overview
This Guidelines summary of British Society for Sexual Medicine guidance provides practical advice on the management of erectile dysfunction in men.
Reflecting on your Learnings
Reflection is important for continuous learning and development, and a critical part of the revalidation process for UK healthcare professionals. Click here to access the Guidelines Reflection Record.
What Is Erectile Dysfunction?
- Erectile dysfunction (ED) is the persistent inability to attain and/or maintain an erection sufficient for satisfactory sexual performance
- ED is caused by various vascular, neuronal, hormonal and metabolic factors, mediated by endothelial and smooth-muscle dysfunction
- Although most causes of ED are physical, some are due to psychosexual issues; nevertheless, all patients with ED should have a history, examination and investigations performed, even if a psychological cause is suspected
- ED is a cardiovascular (CV) risk factor, posing a risk equivalent to that of current, moderate smoking
- ED is also an important marker for future CV events, with symptoms occurring some 3–5 years before an event
- The physical and psychosocial effects of ED can significantly affect the quality of life of patients and their partners
Who is at Risk?
- The risk factors for ED are similar to those for cardiovascular disease (CVD):
- older age
- sedentary lifestyle
- obesity
- dyslipidaemia
- metabolic syndrome
- diabetes
- smoking
What are the Other Benefits of Case-finding ED in Practice?
- Increasing awareness regarding the availability of safe and effective oral drugs for ED, has led to more men seeking help for this condition, which facilitates the early detection of:
- diabetes (ED may be the first symptom in up to 20% of men)
- dyslipidaemia (may not require treatment according to primary prevention guidelines, but may be a major reversible component in ED)
- occult cardiac disease (in an otherwise asymptomatic man, ED may be a marker for underlying coronary artery disease)
- testosterone deficiency (TD; a reversible cause of ED that may not require specific ED treatment, and which also has other long-term health implications)
- associated lower urinary tract symptoms (LUTS)/benign prostatic hyperplasia (BPH) (ED and LUTS severity are closely related, and treatments for one condition may beneficially or adversely affect the other)
| Box 1: Recommendations for History-taking |
|---|
|
| Abbreviations: IIEF=International Index of Erectile Function; SHIM=Sexual Health Inventory for Men; IPSS=International Prostate Symptom Score; AMS=Aging Males’ Symptoms |
| Box 2: Recommendations for Physical Examination |
|---|
|
| Abbreviations: DRE=digital rectal examination; TD=testosterone deficiency |
| Box 3: Recommendations for Investigations |
|---|
|
| Abbreviations: TT=total testosterone; LH=luteinising hormone; FT=free testosterone; TD=testosterone deficiency; SHBG=sex hormone-binding globulin; ED=erectile dysfunction; CV=cardiovascular; PSA=prostate-specific antigen |
Diagnosing and Managing ED in Primary Care
- The primary objective in the management of ED is to enable the man or couple to enjoy a satisfactory sexual experience
- When managing ED, consider not only the efficacy and safety of the different treatments, but also patient and partner preference, and all the factors that may influence this
- It is of paramount importance to use the opportunity to manage any previously undiagnosed comorbidities that present following the patient assessment, and to treat to target any existing conditions and make lifestyle modifications, where necessary
Algorithm 1: Diagnosing and Managing ED in Primary Care
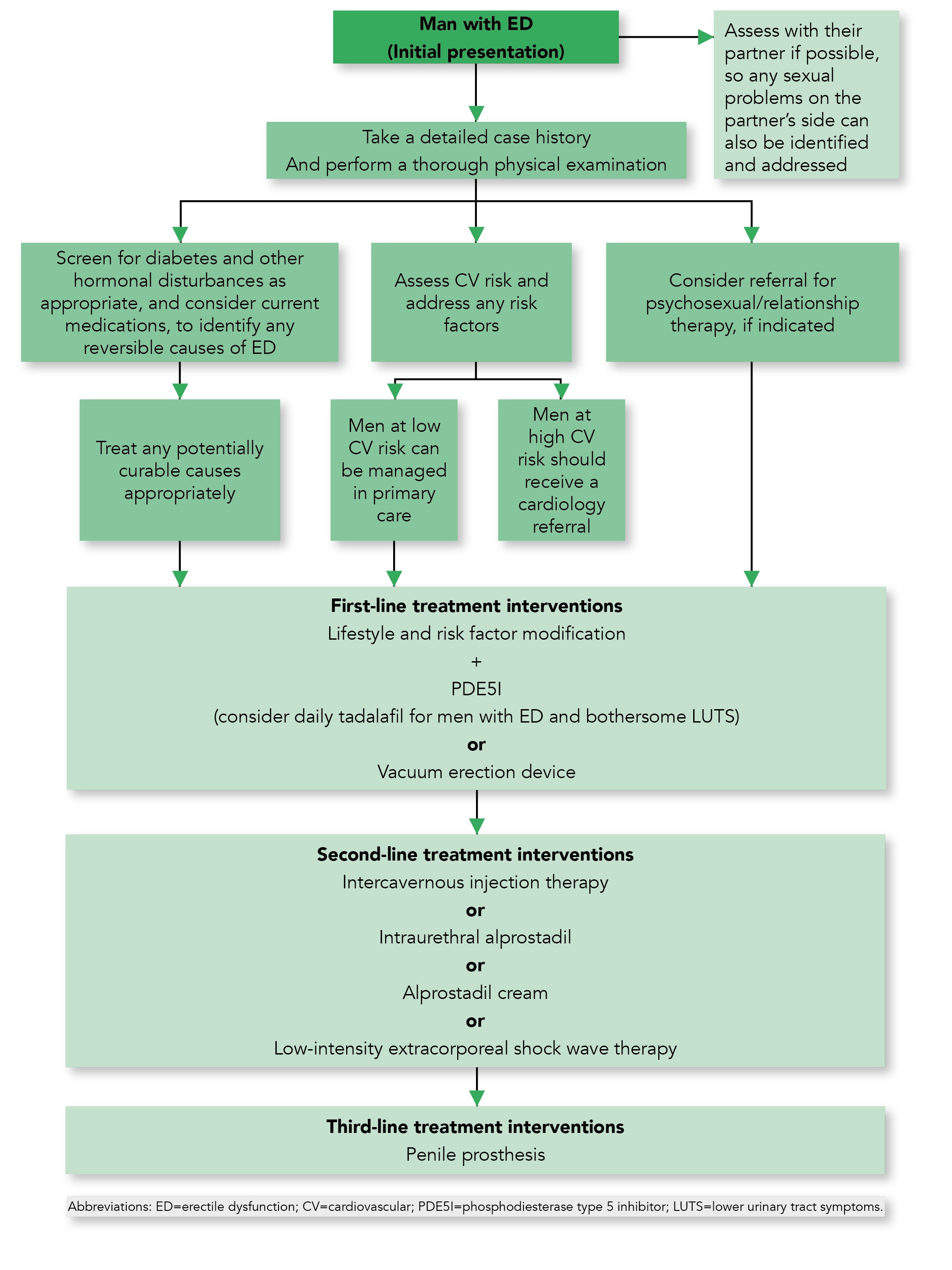
Table 1: Erectile Dysfunction Therapies—Management in Primary Care
| PDE51 | Intra-urethral Alprostadil | Intracavernous Injections | Vacuum Erection Devices | Alprostadil Cream |
|---|---|---|---|---|
Possible adverse effects include:[A]
|
Possible adverse effects include:
|
|
|
Possible adverse effects include:
|
| [A] See the individual Summary of Product Characteristics for full details, because these vary between products. Abbreviations: T2DM=type 2 diabetes mellitus; RP=radical prostatectomy; CYP3A4=cytochrome P450 3A4; NAION=non-arteritic anterior ischaemic optic neuropathy; MUSE=Medicated Urethral System for Erections; ED=erectile dysfunction; PDE5I=phosphodiesterase type 5 inhibitor; IIEF=International Index of Erectile Function | ||||

