Latest Guidance UpdatesOctober 2023: In the section on investigating suspected thyroid dysfunction, NICE added a new recommendation on the potential for biotin to interfere with the results of thyroid function tests. The Guidelines team added the section Managing and monitoring subclinical hypothyroidism, and information on antithyroid drugs for adults, children, and young people with hyperthyroidism in the section Managing thyrotoxicosis. |
Overview
This Guidelines summary covers investigating all suspected thyroid disease and managing primary thyroid disease (related to the thyroid rather than the pituitary gland). This summary only covers information relevant to primary care.
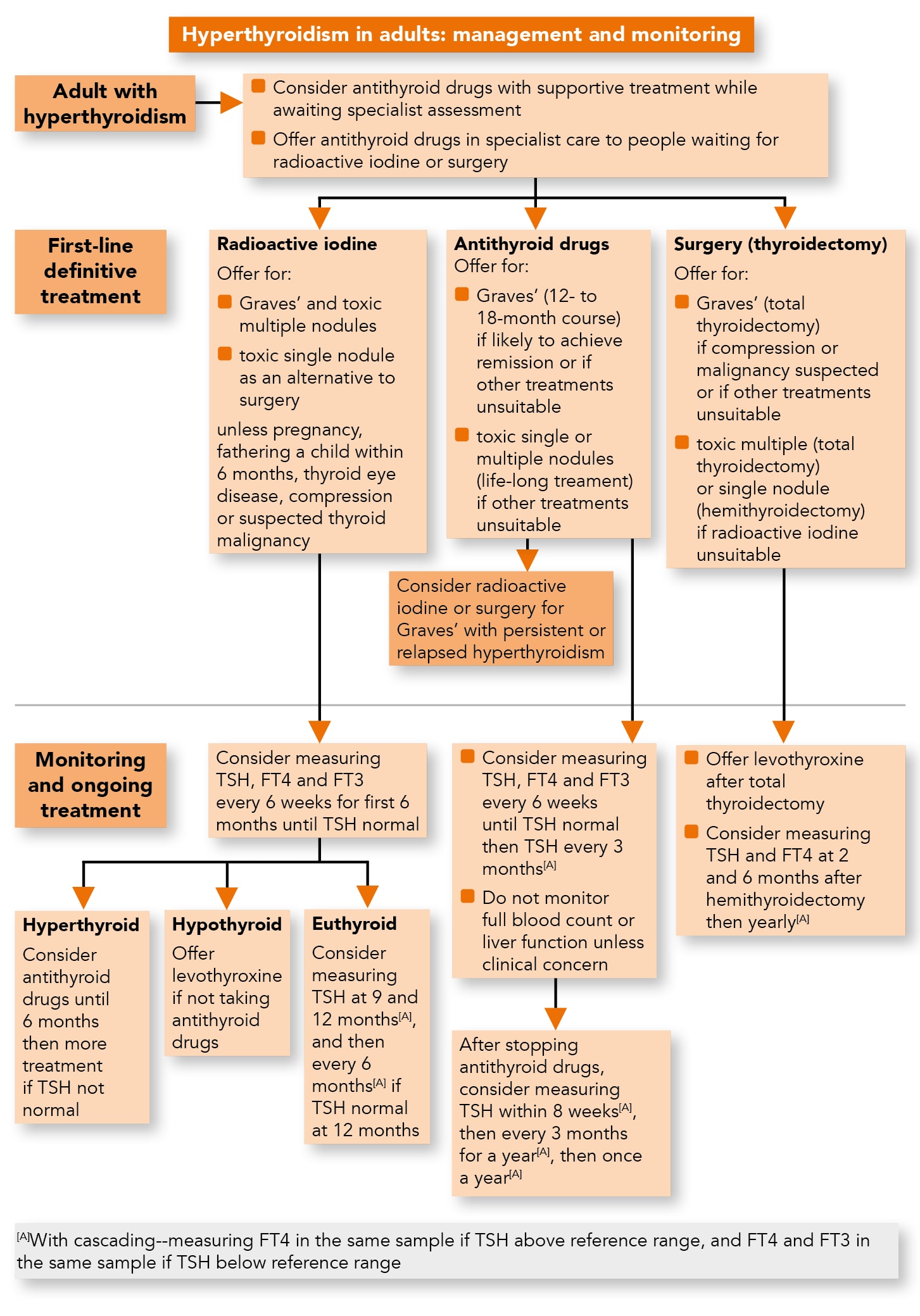
Hyperthyroidism in Adults: Management and Monitoring
Algorithm 1: Management and Monitoring of Hyperthyroidism in Adults
Investigating Suspected Thyroid Dysfunction
Indications for Tests for Thyroid Dysfunction
- Consider tests for thyroid dysfunction for adults, children and young people if there is a clinical suspicion of thyroid disease, but bear in mind that 1 symptom alone may not be indicative of thyroid disease.
- Offer tests for thyroid dysfunction to adults, children and young people with:
- type 1 diabetes or other autoimmune diseases, or
- new-onset atrial fibrillation.
- Consider tests for thyroid dysfunction for adults, children and young people with depression or unexplained anxiety.
- Consider tests for thyroid dysfunction for children and young people with abnormal growth, or unexplained change in behaviour or school performance.
- Be aware that in menopausal women symptoms of thyroid dysfunction may be mistaken for menopause.
- Do not test for thyroid dysfunction during an acute illness unless you suspect the acute illness is due to thyroid dysfunction, because the acute illness may affect the test results.
- Do not offer testing for thyroid dysfunction solely because an adult, child or young person has type 2 diabetes.
Tests when Thyroid Dysfunction is Suspected
- Consider measuring thyroid-stimulating hormone (TSH) alone for adults when secondary thyroid dysfunction (pituitary disease) is not suspected. Then:
- if the TSH is above the reference range, measure free thyroxine (FT4) in the same sample
- if the TSH is below the reference range, measure FT4 and free tri-iodothyronine (FT3) in the same sample.
- Consider measuring both TSH and FT4 for:
- adults when secondary thyroid dysfunction (pituitary disease) is suspected
- children and young people.
If the TSH is below the reference range, measure FT3 in the same sample.
- Consider repeating the tests for thyroid dysfunction in the full guideline if symptoms worsen or new symptoms develop (but no sooner than 6 weeks from the most recent test).
- Ask adults, children and young people with suspected thyroid dysfunction about their biotin intake because a high consumption of biotin from dietary supplements may lead to falsely high or low test results.
Managing Primary Hypothyroidism
Tests for People with Confirmed Primary Hypothyroidism
Adults
- Consider measuring thyroid peroxidase antibodies (TPOAbs) for adults with TSH levels above the reference range, but do not repeat TPOAbs testing.
Children and Young People
- Measure TPOAbs for children and young people with TSH levels above the reference range, with possible repeat TPOAbs testing at the time of transition to adult services.
Managing Primary Hypothyroidism
- Offer levothyroxine as first-line treatment for adults, children and young people with primary hypothyroidism.
- Do not routinely offer liothyronine for primary hypothyroidism, either alone or in combination with levothyroxine, because there is not enough evidence that it offers benefits over levothyroxine monotherapy, and its long-term adverse effects are uncertain.
- Do not offer natural thyroid extract for primary hypothyroidism because there is not enough evidence that it offers benefits over levothyroxine, and its long-term adverse effects are uncertain.
Natural thyroid extract does not have a UK marketing authorisation so its safety is uncertain. - Consider starting levothyroxine at a dosage of 1.6 micrograms per kilogram of body weight per day (rounded to the nearest 25 micrograms) for adults under 65 with primary hypothyroidism and no history of cardiovascular disease.
- Consider starting levothyroxine at a dosage of 25 to 50 micrograms per day with titration for adults aged 65 and over and adults with a history of cardiovascular disease.
Follow-up and Monitoring of Primary Hypothyroidism
Tests for Follow-up and Monitoring of Primary Hypothyroidism
- Aim to maintain TSH levels within the reference range when treating primary hypothyroidism with levothyroxine. If symptoms persist, consider adjusting the dose of levothyroxine further to achieve optimal wellbeing, but avoid using doses that cause TSH suppression or thyrotoxicosis.
- Be aware that the TSH level can take up to 6 months to return to the reference range for people who had a very high TSH level before starting treatment with levothyroxine or a prolonged period of untreated hypothyroidism. Take this into account when adjusting the dose of levothyroxine.
Adults
- For adults who are taking levothyroxine for primary hypothyroidism, consider measuring TSH every 3 months until the level has stabilised (2 similar measurements within the reference range 3 months apart), and then once a year.
- Consider measuring FT4 as well as TSH for adults who continue to have symptoms of hypothyroidism after starting levothyroxine.
Children and Young People Aged 2 Years and Over
- For children aged 2 years and over and young people taking levothyroxine for primary hypothyroidism, consider measuring FT4 and TSH:
- every 6 to 12 weeks until the TSH level has stabilised (2 similar measurements within the reference range 3 months apart), then
- every 4 to 6 months until after puberty, then
- once a year.
Children Under 2 years
- For children aged between 28 days and 2 years who are taking levothyroxine for primary hypothyroidism, consider measuring FT4 and TSH:
- every 4 to 8 weeks until the TSH level has stabilised (2 similar measurements within the reference range 2 months apart), then
- every 2 to 3 months during the first year of life, and
- every 3 to 4 months during the second year of life.
Managing and Monitoring Subclinical Hypothyroidism
Tests for People with Confirmed Subclinical Hypothyroidism
Adults
- Consider measuring TPOAbs for adults with TSH levels above the reference range, but do not repeat TPOAbs testing.
Treating Subclinical Hypothyroidism
- When discussing whether or not to start treatment for subclinical hypothyroidism, take into account features that might suggest underlying thyroid disease, such as symptoms of hypothyroidism, previous radioactive iodine treatment or thyroid surgery, or raised levels of thyroid autoantibodies.
Adults
- Consider levothyroxine for adults with subclinical hypothyroidism who have a TSH of 10 mlU/litre or higher on 2 separate occasions 3 months apart. Follow the recommendations in the section on follow-up and monitoring of hypothyroidism.
- Consider a 6-month trial of levothyroxine for adults under 65 with subclinical hypothyroidism who have:
- a TSH above the reference range but lower than 10 mlU/litre on 2 separate occasions 3 months apart, and
- symptoms of hypothyroidism.
- If symptoms do not improve after starting levothyroxine, re-measure TSH and if the level remains raised, adjust the dose. If symptoms persist when serum TSH is within the reference range, consider stopping levothyroxine and follow the recommendations on monitoring untreated subclinical hypothyroidism and monitoring after stopping treatment.
Children and Young People Aged 2 Years and Over
- Consider levothyroxine for children aged 2 years and over and young people with subclinical hypothyroidism who have:
- a TSH level of 20 mlU/litre or higher, or
- a TSH level between 10 and 20 mlU/litre on 2 separate occasions 3 months apart, or
- a TSH level between 5 and 10 mlU/litre on 2 separate occasions 3 months apart, and
- thyroid dysgenesis (an underdeveloped thyroid gland), or
- signs or symptoms of thyroid dysfunction.
During levothyroxine treatment, follow the recommendations in the section on follow-up and monitoring.
Children Under 2 Years
- Consider levothyroxine for children aged between 28 days and 2 years with subclinical hypothyroidism who have a TSH level of 10 mlU/litre or higher. During levothyroxine treatment, follow the recommendations in the section on follow-up and monitoring.
Monitoring Untreated Subclinical Hypothyroidism and Monitoring After Stopping Treatment
Adults
- For adults with untreated subclinical hypothyroidism or adults who have stopped levothyroxine treatment for subclinical hypothyroidism, consider measuring TSH and FT4:
- once a year if they have features suggesting underlying thyroid disease, such as previous thyroid surgery or raised levels of thyroid autoantibodies, or
- once every 2 to 3 years if they have no features suggesting underlying thyroid disease.
Children and Young People
- Consider measuring TSH and FT4 for children aged 2 years and over and young people with untreated subclinical hypothyroidism and a TSH lower than 10 mlU/litre:
- every 3 to 6 months if they have features suggesting underlying thyroid disease, such as thyroid dysgenesis (an underdeveloped thyroid gland) or raised levels of thyroid autoantibodies, or
- every 6 to 12 months if they have no features suggesting underlying thyroid disease.
- Consider measuring TSH and FT4 every 1 to 3 months for children aged between 28 days and 2 years with untreated subclinical hypothyroidism.
- Consider stopping TSH and FT4 measurement in children and young people if the TSH level has stabilised (2 similar measurements within the reference range 3 to 6 months apart) and there are no features suggesting underlying thyroid disease.
Managing Thyrotoxicosis
Tests for People with Confirmed Thyrotoxicosis
Adults
- Differentiate between thyrotoxicosis with hyperthyroidism (for example, Graves’ disease or toxic nodular disease) and thyrotoxicosis without hyperthyroidism (for example, transient thyroiditis) in adults by:
- measuring TSH receptor antibodies (TRAbs) to confirm Graves’ disease
- considering technetium scanning of the thyroid gland if TRAbs are negative.
- Only consider ultrasound for adults with thyrotoxicosis if they have a palpable thyroid nodule.
Children and Young People
- Differentiate between thyrotoxicosis with hyperthyroidism (Graves’ disease) and thyrotoxicosis without hyperthyroidism (for example, transient thyroiditis) in children and young people by:
- measuring TPOAbs and TRAbs
- considering technetium scanning of the thyroid gland if TRAbs are negative.
- Only offer ultrasound to children and young people with thyrotoxicosis if they have a palpable thyroid nodule or the cause of thyrotoxicosis remains unclear following thyroid autoantibody testing and technetium scanning.
Initial Treatment in Primary/Non-specialist Care
- Be aware that transient thyrotoxicosis without hyperthyroidism usually only needs supportive treatment (for example, beta-blockers).
- Consider antithyroid drugs along with supportive treatment for adults with hyperthyroidism who are waiting for specialist assessment and further treatment.
Use of carbimazole is subject to MHRA advice on contraception (Drug Safety Update, February 2019) and risk of acute pancreatitis (Drug Safety Update, February 2019).
Antithyroid Drugs for Adults, Children and Young People with Hyperthyroidism
- Before starting antithyroid drugs for adults, children and young people with hyperthyroidism, check full blood count and liver function tests.
- When offering antithyroid drugs as first-line definitive treatment to adults with Graves' disease, offer carbimazole for 12 to 18 months, using either a block and replace or a titration regimen, and then review the need for further treatment.
Use of carbimazole is subject to MHRA advice on contraception (Drug Safety Update, February 2019) and risk of acute pancreatitis (Drug Safety Update, February 2019). - When offering antithyroid drugs to children and young people with Graves' disease, offer carbimazole, using a titration regimen, and review the need for treatment every 2 years.
Use of carbimazole is subject to MHRA advice on contraception (Drug Safety Update, February 2019) and risk of acute pancreatitis (Drug Safety Update, February 2019). November 2019 – carbimazole use is off label for children under 2 years. See NICE's information on prescribing medicines. - When offering life-long antithyroid drugs to adults with hyperthyroidism secondary to a single or multiple toxic nodules, consider treatment with a titration regimen of carbimazole.
- Consider propylthiouracil for adults:
- who experience adverse reactions to carbimazole
- who are pregnant or trying to become pregnant within the following 6 months
- with a history of pancreatitis.
- Stop and do not restart any antithyroid drugs if a person develops agranulocytosis. Consider referral to a specialist for further management options.
Follow-up and Monitoring of Hyperthyroidism
Monitoring after Radioactive Iodine Treatment
- Consider measuring TSH, FT4 and FT3 levels in adults, children and young people every 6 weeks for the first 6 months after radioactive iodine treatment until TSH is within the reference range.
- For adults, children and young people who have hypothyroidism after radioactive iodine treatment and are not on antithyroid drugs, offer levothyroxine replacement therapy and follow recommendations in ‘Managing primary hypothyroidism’ on dosage of levothyroxine for adults and in ‘Tests for follow-up and monitoring of primary hypothyroidism’ on monitoring of hypothyroidism.
- For adults, children and young people with TSH in the reference range 6 months after radioactive iodine treatment, consider measuring TSH (with cascading) at 9 months and 12 months after treatment.
- For adults, children and young people with TSH in the reference range 12 months after radioactive iodine treatment, consider measuring TSH (with cascading) every 6 months unless they develop hypothyroidism (then follow the recommendation above).
- If hyperthyroidism persists after radioactive iodine treatment in adults, children and young people, consider antithyroid drugs until the 6-month appointment.
Use of carbimazole is subject to MHRA advice on contraception (Drug Safety Update, February 2019) and risk of acute pancreatitis (Drug Safety Update, February 2019). November 2019 – carbimazole use is off label for children under 2 years. See NICE's information on prescribing medicines. - If hyperthyroidism persists 6 months after radioactive iodine treatment in adults, children and young people, consider further treatment.
Monitoring of Antithyroid Drugs
- For adults, children and young people who are taking antithyroid drugs for hyperthyroidism, consider measuring:
- TSH, FT4 and FT3 every 6 weeks until their TSH is within the reference range, then
- TSH (with cascading) every 3 months until antithyroid drugs are stopped.
- Do not monitor full blood count and liver function for adults, children and young people taking antithyroid drugs for hyperthyroidism unless there is a clinical suspicion of agranulocytosis or liver dysfunction.
- For adults who have stopped antithyroid drugs, consider measuring:
- TSH (with cascading) within 8 weeks of stopping the drug, then
- TSH (with cascading) every 3 months for a year, then
- TSH (with cascading) once a year.
- For children and young people who have stopped antithyroid drugs, consider measuring:
- TSH, FT4 and FT3 within 8 weeks of stopping the drug, then
- TSH, FT4 and FT3 every 3 months for the first year, then
- TSH (with cascading) every 6 months for the second year, then
- TSH (with cascading) once a year.
Managing and Monitoring Subclinical Hyperthyroidism
Treating Subclinical Hyperthyroidism
- Consider seeking specialist advice on managing subclinical hyperthyroidism in adults if they have:
- 2 TSH readings lower than 0.1 mIU/litre at least 3 months apart and
- evidence of thyroid disease (for example, a goitre or positive thyroid antibodies) or symptoms of thyrotoxicosis.
- Consider seeking specialist advice on managing subclinical hyperthyroidism in all children and young people.
Untreated Subclinical Hyperthyroidism
- Consider measuring TSH every 6 months for adults with untreated subclinical hyperthyroidism. If the TSH level is outside the reference range, consider measuring FT4 and FT3 in the same sample.
- Consider measuring TSH, FT4 and FT3 every 3 months for children and young people with untreated subclinical hyperthyroidism.
- Consider stopping TSH measurement for adults, children and young people with untreated subclinical hyperthyroidism if the TSH level stabilises (2 similar measurements within the reference range 3 to 6 months apart).
For information on diagnosing, managing and monitoring thyroid enlargement with normal thyroid function, see the full guideline.

