Overview
This guideline only covers symptomatic, chronic forms of prostatitis; that is, chronic bacterial prostatitis (CBP) (NIH category II) and chronic prostatitis (CP)/chronic pelvic pain syndrome (CPPS) (NIH category III).
A diagnosis of CBP (NIH category II) or CP/CPPS (NIH category III) should be based on a history of persistent or recurrent symptoms, and the absence of other urogenital pathology (for example, active urethritis, urogenital cancer, urinary tract disease), for a minimum of 3 out of the past 6 months.
Priorities for Implementation
- Patients with CBP or CP/CPPS should be managed according to their individual symptom pattern—no single management pathway is suitable for all patients with these conditions (see treatment algorithm and table)
- Most patients with CP/CPPS do not have an infection, and repeated use of antibiotics such as quinolones should be avoided where no obvious benefit from infection control is evident or cultures do not support an infective aetiology
- Early use of antineuropathic pain medication should be considered for all CBP and CP/CPPS patients refractory to initial treatments. If neuropathic pain is suspected, ensure a quick referral to the multidisciplinary team (MDT), which includes pain specialists
- Early referral to specialist services should be considered when patients fail to respond to initial measures. Referral should ideally be to a clinician with an interest in the management of CBP and/or CP/CPPS, but not necessarily a urologist
- An MDT approach should be implemented and made available to CBP and CP/CPPS patients. The MDT should include urologists, pain specialists, nurse specialists, specialist physiotherapists, GPs, cognitive behavioural therapists/psychologists and sexual health specialists
- Patients should be fully informed about the possible underlying causes and treatment options of CBP and CP/CPPS. The MDT responsible for the management of these patient groups, should be able to explain the chronic pain cycle and other relevant information to improve patient understanding of the conditions.
Diagnosis and Management of CBP and CP/CPPS
Algorithm 1: Algorithm for Diagnosis and Management of CBP and CP/CPPS
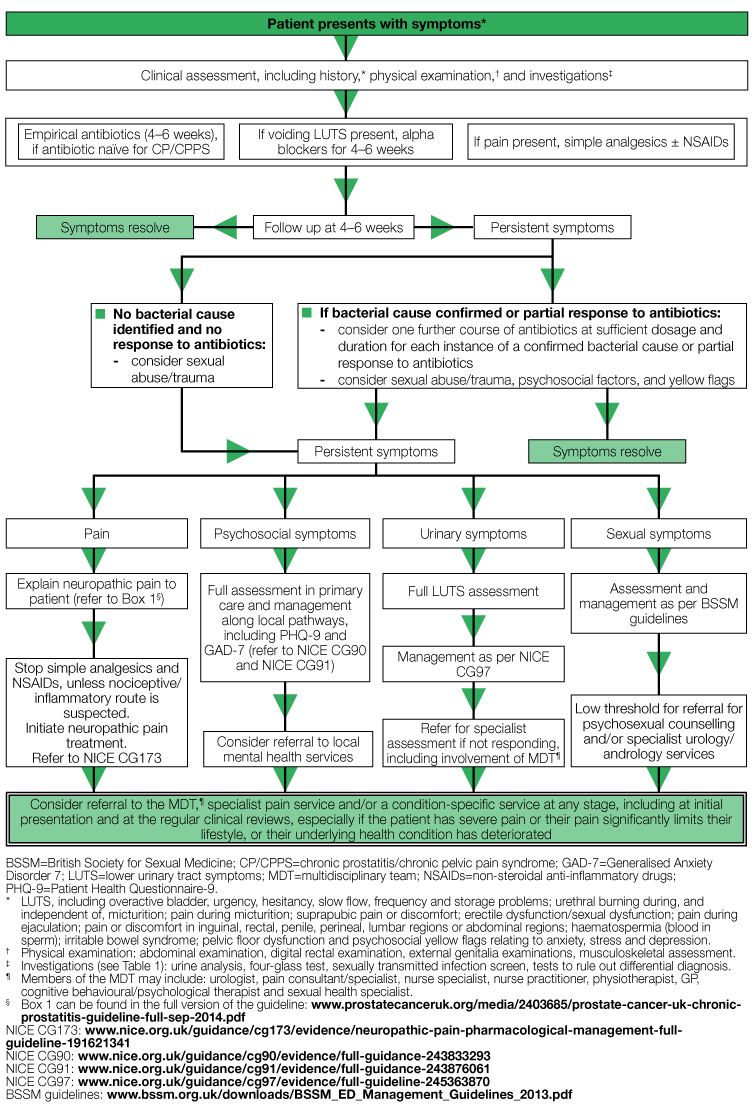
* LUTS, including overactive bladder, urgency, hesitancy, slow flow, frequency and storage problems; urethral burning during, and independent of, micturition; pain during micturition; suprapubic pain or discomfort; erectile dysfunction/sexual dysfunction; pain during ejaculation; pain or discomfort in inguinal, rectal, penile, perineal, lumbar regions or abdominal regions; haematospermia (blood in sperm); irritable bowel syndrome; pelvic floor dysfunction and psychosocial yellow flags
relating to anxiety, stress and depression.
† Physical examination: abdominal examination, digital rectal examination, external genitalia examinations, musculoskeletal assessment.
‡ Investigations (see Table 1): urine analysis, four-glass test, sexually transmitted infection screen, tests to rule out differential diagnosis.
¶ Members of the MDT may include: urologist, pain consultant/specialist, nurse specialist, nurse practitioner, physiotherapist, GP, cognitive behavioural/psychological therapist and sexual health specialist.
§ Box 1 can be found in the full version of the guideline: www.prostatecanceruk.org/media/2403685/prostate-cancer-uk-chronic-prostatitis-guideline-full-sep-2014.pdf
NICE CG173: www.nice.org.uk/guidance/cg173/evidence/neuropathic-pain-pharmacological-management-full-guideline-191621341
NICE CG90: www.nice.org.uk/guidance/cg90/evidence/full-guidance-243833293
NICE CG91: www.nice.org.uk/guidance/cg91/evidence/full-guideline-243876061
NICE CG97: www.nice.org.uk/guidance/cg97/evidence/full-guideline-245363870
BSSM guidelines: www.bssm.org.uk/downloads/BSSM_ED_Management_Guidelines_2013.pdf
Table 1. Summary of Physical Examinations and Investigations to Consider During the Clinical Assessment of CBP and CP/CPPS
| Setting | Rating | |||
|---|---|---|---|---|
| Examinations and Investigations* | Non-specialist | Specialist | Core | Optional |
Physical examinations: Digital rectal examination
| ✓ | ✓ | ✓ | |
Abdomen
| ✓ | ✓ | ✓ | |
| Urine dipstick and/or MSU for culture/microscopy | ✓ | ✓ | ✓ | |
Four-glass or two-glass test† VB1—voided bladder
EPS—expressed prostatic secretions
| ✓ | ✓ | ||
| Tests to rule out differential diagnoses:‡ | ||||
| PSA testing to exclude prostate cancer | ✓ | ✓ | ✓ | |
| STI screen (e.g. via NAATs) | ✓ | ✓ | ✓ | |
| Uroflowmetry, retrograde urethrography or cystoscopy (to exclude BOO, urethral stricture or bladder neck stenosis | ✓ | ✓ | ||
| Prostate biopsy (only if prostate cancer is suspected on basis of PSA and/or DRE results | ✓ | ✓ | ||
| Transrectal ultrasound (only in refractory patients in whom a prostatic abscess or other pathology is suspected) | ✓ | ✓ | ||
| Diagnostic cystoscopy if bladder cancer is suspected | ✓ | ✓ | ||
| Urethral swab and culture if urethritis is suspected | ✓ | ✓ | ||
| MRI if prostatic abscess suspected | ✓ | ✓ | ||
| * Based on information adapted from Map of Medicine, Prostatitis—Primary Care, January 2014, Map of Medicine, Prostatitis—Secondary Care, January 2014, Nickel et al, 2003, and PERG consensus † Pursued when CBP is suspected ‡ The investigations pursued will depend on symptom presentation and patient history. N.B. Local provider services may vary with respect to the division of assessment options across non-specialist and specialists settings. BOO=bladder outlet obstruction; CBP=chronic bacterial prostatitis; CP/CPPS=chronic prostatitis/chronic pelvic pain syndrome; MRI=magnetic resonance imaging; MSU=midstream urine; NAATs=nucleic acid amplification tests; PSA=prostate-specific antigen; STI=sexually transmitted infection | ||||
Antibiotic Treatment Options
- Quinolones, e.g. ciprofloxacin—consider first-line
- Trimethoprim—consider second-line
- Tetracyclines, e.g. doxycycline—consider second-line
- Macrolides, e.g. azithromycin—reserve for special indications.
Treatment Options for Neuropathic Pain
- Gabapentinoids:
- gabapentin
- pregabalin
- Tricyclic antidepressants/serotonin–norepinephrine reuptake inhibitors:
- amitriptyline
- duloxetine.

